Of all the potential injuries a runner may incur, plantar foot pain may be the most feared. It is painful and debilitating, and the recovery time can be months or years.
Of all the potential injuries a runner may incur, plantar foot pain may be the most feared. It is painful and debilitating, and the recovery time can be months or years.
Why do some injuries, like this one where pain is seemingly felt in the plantar fascia, take longer to heal than others? Perhaps it is the tissue type. By nature, fascia is dense and tight, with low blood flow, and the forces through our feet while running are unavoidable.
But there may be other reasons why overcoming plantar foot pain is so challenging and frustrating. First, what often hurts isn’t actually the plantar fascia, which we covered years ago in our plantar fasciitis article. More importantly, we often don’t recognize and correct the root cause of the issue.
A few columns ago, we introduced Joe’s Fix-It Series. Our intention with this series is not to regurgitate basic information easily found online. Rather, it is to provide a lifeline to frustrated runners who have tried all the advice and treatments, both online and in-person, yet continue to struggle with certain injuries.
The goal of Joe’s Fix-It Series is to share lessons I have learned the hard way — through clinical experimentation and personal frustration as a veteran orthopedist, coach, and runner — on those crucial pieces of injury treatment still missing. In this case, we explore:
- What exactly hurts in our foot
- Why it hurts
- A comprehensive, whole-body way to heal it
All the articles in Joe’s Fix-It Series are constructed similarly. To learn more, see our series introduction.

We hope this article can help you run pain-free and with joy through scenes like this, of iRunFar’s Hannah Green weaving through aspen trees on a Colorado trail run. Photo: iRunFar/Eszter Horanyi
Plantar Foot Pain Introduction
Plantar fasciitis is an irritation or strain of the plantar fascia, the thick band of connective tissue extending from the heel bone to the toes. This structure serves as a shock absorber and energy-return mechanism in the foot. Overload can lead to strain, and a strained plantar fascia may result in plantar foot tightness, sharp heel or arch pain, morning stiffness, pain during and after running, and even standing and walking limitations.
Conventional wisdom says that plantar fascia pain may result from running too far, too fast, and/or too quickly. Or running with an inefficient foot strike. Or increasing tightness in the foot and lower leg from a lot of running, putting excess strain on the plantar fascia.
The keys to plantar fascia healing include rest by cutting running volume or stopping entirely. Support — including orthotics, stiffer shoes, and/or taping — may also be helpful. Mobility strategies include massage and stretching of the plantar foot. Strength exercises for the calf, ankle, and foot can help support and strengthen the plantar fascia. Stride optimization by avoiding either excessive heel or forefoot landing in the running stride may help relieve foot stress.
Mild strains tend to heal within three weeks, with more moderate or severe cases requiring six to 12 weeks of significant rest. This is followed by a gradual resumption of running, via a ramping up of volume, speed, and terrain difficulty.
Sounds simple and straightforward, right? Then why do most cases of what presents as plantar foot pain hardly ever play out this simply?
What It Is Versus What Else It Could Be
The major factor in the slow or stalled recovery from plantar foot pain is not the plantar fascia. The foot and ankle have many structures, including bones, joints, and nerves, all of which can hurt and may require a different approach for healing.
- Bones and joints: These include the calcaneus and talus (subtalar joint), talus and navicular (talonavicular joint), cuneiforms, and cuboid.
- Myofascial structures: In addition to the plantar fascia, other tissues susceptible to strain include the posterior tibialis, flexor digitorum and flexor hallucis muscles and tendons, medial foot and ankle ligaments, and intrinsic foot muscles.
- Nerves: Several nerves can cause — or amplify and sustain — plantar foot pain, including the medial plantar, tibial, sural, and sciatic nerves.
- Fat pad: The calcaneal fat pad can cause stubborn heel pain. This is often because it loses mobility, and the small sensory nerves that flow into it from the medial plantar nerve get stuck.

Plantar foot pain has many possible causes, so be sure to investigate the root of yours before developing a treatment plan so you can get back on the trail sooner. Photo: iRunFar/Eszter Horanyi
Causes of Plantar Foot Pain
In my opinion, the bigger reason that plantar foot pain can take so long to get better is that we often fail to recognize and treat the root cause. Here we discuss several factors that contribute to plantar foot pain. It only takes one, but in many cases — particularly the most stubborn ones — several factors are present.
We want to note a causal factor that is underappreciated by runners and sports medicine professionals alike, derived from my three laws of running injury: A push-off deficit in one leg will cause a compensatory landing on the other leg. That is, if any aspect of the push-off leg underperforms, the swing-through leg must compensate, usually in the form of an overreach. In doing so, the resultant foot strike is more stressful, which is often cited as a potential cause of foot pain.
Overuse and/or Doing Something Different
In my experience, running too far or too fast or on different terrain may be minor factors, but are seldom the only ones. Occasionally, runners who make a drastic change in footwear, terrain, and/or speedwork will strain their plantar foot.
Mobility Deficits
Mobility deficits are far more common. While stiffness in the plantar foot can be a factor, mobility loss elsewhere in the kinetic system is more likely to cause and perpetuate ongoing strain to the foot.
- Foot and ankle: The loss of ankle dorsiflexion and toe extension causes same-sided plantar foot strain through inefficient loading. Motion loss on one foot may also lead to a push-off deficit, which will cause a compensatory over-reach and stressful landing effect on the other, painful foot.
- Hip: The hip is the drive train of our running stride. It must fully and efficiently flex and extend. Hip extension loss on the same side may result in a painful foot, overworking to compensate. Hip extension loss on the opposite side may cause an overreach, over-stride landing on the painful side. A hip flexion deficit has the same effect. If the hip cannot flex upward, the leg often reaches forward instead of upward, resulting in over-stride stress. A loss of hip and pelvic abduction mobility can cause narrow, crossover landing that mimics hyper-pronation.
- Spine: Spinal motion inefficiency can directly or indirectly result in foot pain. Overt stiffness in the thoracic spine, affecting the deep fascia around the diaphragm, can cause hip mobility loss and foot stress effects. Dysfunction anywhere else, particularly the lumbosacral levels, but even the neck, can result in nerve irritation and tension that refers to the lower leg and foot.
- Fascia: Besides the plantar fascia, multiple layers of fascia in the lower leg area can cause both plantar fascial and nerve tension.
Strength Deficits
Weakness in the running system, not just the foot, can result in plantar foot strain.
- Foot and lower leg: The lower leg needs to stay strong upon landing. The foot and ankle muscles and tendons must be strong to moderately pronate without excess arch collapse. Above, the ankle and the knee must stay strong, avoiding excessive flexion from landing to mid-stance. A lack of mid-stance stability, what I refer to as deflating, can cause over-stretch strain with each foot strike.
- Hips: Deficits in the same-side hip flexors can cause an overreaching, stressful landing. Weakness in the bilateral hip extensors (glutes) can either cause the foot to overwork to push off, or the opposite leg to overreach to make up the propulsive difference. Weak lateral hip muscles can cause foot strike faults — including overpronation and crossover landing patterns — that strain the plantar foot.

Good mobility and strength are necessary components for injury-free trail running. Photo: iRunFar/Eszter Horanyi
Efficiency Deficits
Finally, how we run plays a major role in foot pain. Though driven largely by mobility and strength, beyond that, some runners simply have habits that result in excessive foot strain.
- Posture: Deficient hip hinge or excessive spinal extension postures are major factors in foot strain. Either issue can affect rearward propulsion, forward momentum, and efficient foot-under-body landing.
- Over-stride landing: Any time the foot lands significantly in front of the body, excessive force is absorbed somewhere in the kinetic system. This often occurs at the first point of contact with the ground, the foot. While this is largely driven by posture, some runners simply overreach, running with a horizontal hip strategy instead of a vertical one.
- Foot overuse: Lastly, runners occasionally run with an excessive forefoot strike, never allowing their heel to touch the ground. This relentless forefoot load stresses the plantar foot structures. Occasionally, runners over-push-off with their foot and ankle, which creates calf and foot myofascial overuse, as well.
Step 1: What Is It?
Determining the painful tissue isn’t easy. In fact, lots of trained professionals get this wrong, especially if they do not conduct a thorough history and examination, including a running stride assessment. Our original article on plantar foot pain differential diagnosis is a great starting point, and if you follow the systems-based treatment approach, most plantar foot pain will improve.
Nerve pain may require a more specific approach. To help determine if your foot pain might be neurogenic, check out these previous iRunFar articles: Six Signs of Nerve Pain in Runners and Three Types of Nerve Pain.
The better you understand the specific tissues involved, the better your chances of a fast and sustained recovery.
Step 2: Mobility Strategies
On the theme of Joe’s Fix-It Series, while massaging and stretching the painful area may be helpful, mobility strategies must go beyond the foot for sustained pain relief and full recovery. The fix-it plan includes strategies for the:
- Hip and pelvis
- Ribcage and spine
- Foot and ankle
- Nervous system
Hip and Pelvis
Let’s begin at the pelvis and hip, the most frequently overlooked factor in chronic foot pain. Restoring full hip mobility is a crucial step in relieving foot stress.
- Self-massage: Free the pelvis and hip by working the soft tissues around these bones. Use a tennis, lacrosse, or custom-made massage ball to soften the myofascial tissue around the pelvic rim. Then work the hip joint, where the thigh meets the pelvis, in all directions: front (hip flexors), outside and back (glutes), and inside (adductors). See our article on hip self-massage for more.

The author showing the location of the pelvic rim, or where to concentrate self-massage of the hip and pelvis. All photos iRunFar/Joe Uhan unless otherwise mentioned.
- Stretches: Try these three key stretches to restore hip and pelvic mobility.
- Hurdler stretch, discussed in our hip abduction/rotation article
- Boogie board and side lunge, or ninja pose, as seen in our pelvic mobility article
- The runner’s lunge, which is by far the most important because it promotes full hip flexion and extension in the running pattern
Ribcage and Spine
The spine requires full, pain-free, and balanced mobility for efficient running posture and a healthy, mobile nervous system. The ribcage has fascial connections, primarily via the diaphragm, to the pelvis and hips. Keeping both mobile is a crucial yet oft-overlooked component of plantar foot health.
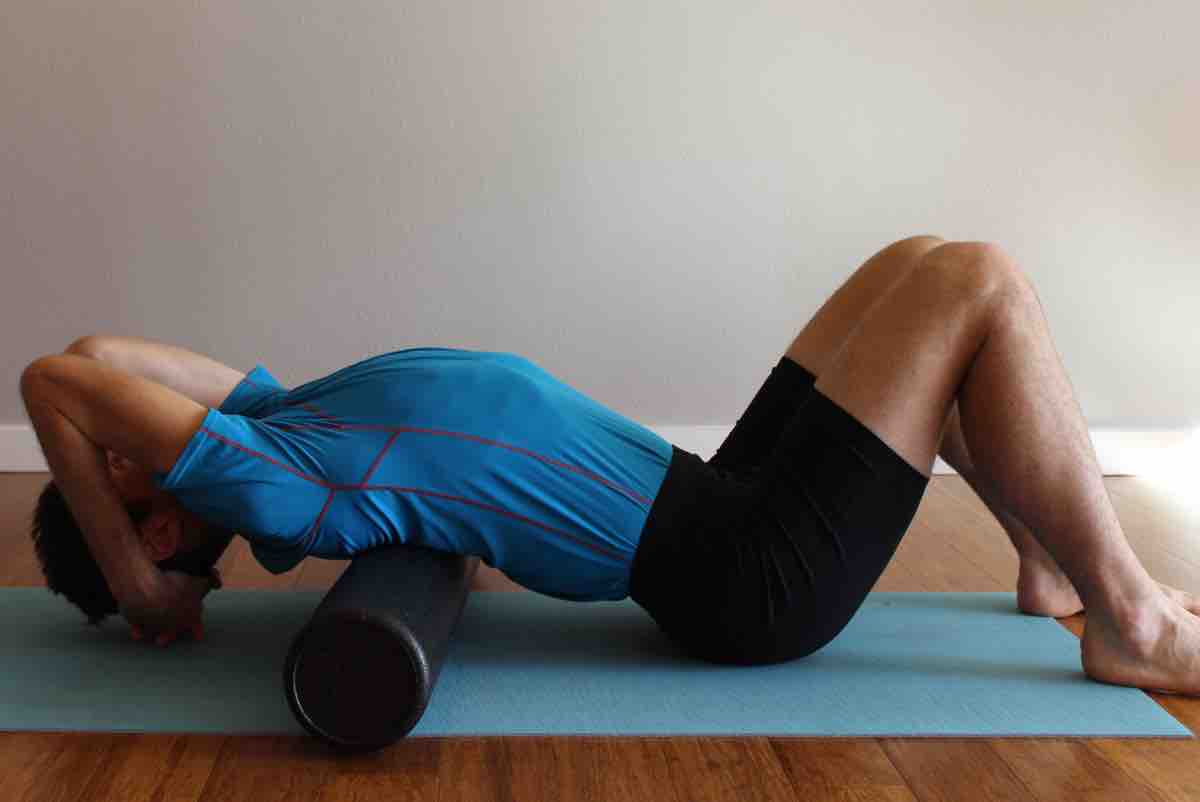
- Foam roll mobilization: Performing multi-dimensional mobility of the ribcage is easy with the foam roll. First, try conventional rolling, followed by prolonged pressure around the diaphragm on both the sides and back, and even the front! An emphasis on trunk and leg rotation will help even out any downstream hip imbalances.
- Stretches: Basic spinal stretching goes a long way to improve both vertebral and nervous system mobility. Classics such as prone extension (the upward dog pose in yoga) and flexion (child’s pose) are great, easy, and pain-free tools. For detailed information, see our article on spinal extension mobility. My favorite thoracic spine and ribcage stretch is this technique using a therapy ball. This stretch promotes elongation and rotation in the running pattern.
Foot and Ankle
- Self-massage: Soft tissue mobilization is a classic strategy for plantar fasciitis, but be careful! For most tissue strains, over-stretch is the injury mechanism. Especially early in the healing process, avoid aggressive self-massage strategies directly on the painful area. Instead, work the entire plantar foot, seeking out and mobilizing any stiff areas adjacent to the painful area. Because fascia is interconnected, self-massaging all surrounding areas — with a ball, foam roll, or other tools — is likely to provide beneficial tissue unloading slack to the painful plantar foot area. This includes all aspects of the plantar foot, Achilles tendon, calf, and medial and lateral shins. Lastly, wiggle free that calcaneal fat pad! Often a sneaky source of heel pain, it is often quickly relieved by grasping the very fleshy bottom of the heel and wiggling it side to side and forward and back. Nerves get impinged on the medial side, and if it is exquisitely tender there and replicates your heel pain, gently continue wiggling the fat pad in every direction until it moves better and soreness decreases!
- Stretches: The foot and ankle must have full motion to unload any strained areas of the foot. Key stretches include:
- Ankle dorsiflexion can be very limited and stubborn to conventional stretching. This belt stretch effectively restores dorsiflexion motion to the ankle joint.
- A toes-on-wall strategy is a great way to work on big toe extension, which is crucial for efficient running.
- Performing a fascial mobilization to the outermost layer of fascia of the foot — via the toes and the lower leg — is a potent way to restore motion and provide slack to the plantar foot. Additionally, since most of the nerves of the lower leg and foot emerge from the superficial fascia, this is a great starting point for nerve mobilization. For a primer on foot and lower leg superficial fascia mobilization, check out our article on the toe spreaders and sock pull exercises.

Stretching your toes on the wall can help with the extension of the big toe. Photo: iRunFar/Eszter Horanyi
Nervous System
Lastly, enhance nervous system mobility in the lower leg and foot. Spinal and ribcage stretching is a key starting point, and superficial fascial mobilizations help free the nerves locally.
- Stretches: Try these two standing sciatic nerve stretches for a stretch targeting the specific nerves of the lower leg and foot.
Step 3. Strength and Stability
Because of its systems-based nature, strength is a crucial element in solving stubborn foot pain. Let’s talk about the key elements to address.
Hips and Core
- Exercises: An activated core enables neutral posture and strong hips.
- If you haven’t tried the diagonal chop exercise, it’s still the best running-specific deep core activator out there.
- Don’t sleep on the hip flexors! A strong, efficient, and vertical hip strategy requires the strongest hip flexors. Work them in supine, a plank, and standing. Then work the early range off a bench or box.
- Work the hip in three dimensions! In addition to standing foot and ankle balance, work the hip abductors and deep stabilizers with the ice skater exercise.
- Stretches: Hip extension is a critical element in foot pain recovery. Start small with bridging — bent knee hip extension in supine. Don’t forget the hamstrings’ role in hip extension, and try these advanced bridges engaging both the glutes and hamstrings.
Foot and Ankle
- Exercise: Shore up essential plantar foot and ankle strength in a running-specific exercise using the runner heel raise plus toe-up exercise. A good goal is at least 25 single-leg raises per side.
- Plyometrics: Light hopping is a critical element for plantar foot injury recovery. Besides supplying a key stimulus to healing connective tissue, being able to quickly hop while maintaining only a slight ankle and knee flexion is a key to efficient landing. A few low-intensity, highly effective hopping exercises can be found in this plyometrics article. Then put it all together with this quick-switch hop, the 100-up exercise.
Step 4: Running Efficiency
Stride efficiency is the next component of plantar foot pain relief and prevention. The foot should land centered, beneath the body, using the whole foot. We offer a few considerations:
- Neutral spine posture, to facilitate an efficient foot strike and avoid spinal and nerve stress
- Forward orientation using a light hip hinge
- To prevent an over-stride landing, use a vertical hip strategy, with emphasis on upward leg lift and a push-off beneath and behind
- To avoid over-pushing with the foot, consider a pull-push drill, such as the pawback, to emphasize both foot-under-body landing and a strong rearward push-off

Trail running around sunset on California singletrack, while demonstrating an efficient stride. Photo: iRunFar/Eszter Horanyi
Step 5: Returning to Running
A comprehensive treatment strategy that addresses system mobility, strength, and efficiency often results in rapid improvement, even after months of stubborn pain. However, if pain is both severe and more acute, consider the following unloading strategies:
- Stiffer shoes that have minimal flex or torsional flexibility
- Plantar foot taping, using kinesiology, athletic, or medical tape
- Braces, including walking boots and night splinting
When you can walk and stand for normal periods with minimal pain, you can begin a return-to-run program. Here are some guidelines:
- Consider wearing stiffer running shoes for the initial return to running.
- Initial running should be on flat, mostly even, smooth, and firm surfaces. Avoid terrain that is too soft, as this may over-stress the plantar foot structures.
- Avoid hilly running until you can run on flat, even surfaces for four to five miles with minimal pain.
Once you have progressed to continuous running, several times a week, it is time to add a comprehensive load. This may include:
- Softer footwear
- Hilly terrain
- Very short periods of barefoot walking and then barefoot running
- Dynamic speedwork, such as short build-up sprints
Conclusion
Overcoming plantar foot pain demands a comprehensive strategy that addresses not just the symptomatic area but the entire kinetic chain — from mobility and strength deficits to running efficiency. This whole-body approach can deliver swift pain relief and lasting recovery, even for cases lingering months or years, by targeting overlooked root causes and restoring balanced function. Get to work!
Call for Comments
- Have you experienced or do you now have plantar foot pain? Were you able to determine the root cause?
- Have you given any of these exercises a try for your plantar foot pain?
Disclaimer
All medical advice found online is for educational purposes only, including in this article. It is not intended to diagnose or treat yours or any other specific illness, injury, or dysfunction. All readers should consult with a licensed medical professional as to whether these approaches are safe and appropriate for their specific needs.