 It wasn’t that long ago when runners had scant options to address stiffness, aches, and myofascial pain. Only a few decades ago, there were no foam rollers or massage sticks, let alone the fancy gadgets designed to mobilize the stressed and strained muscles of endurance athletes.
It wasn’t that long ago when runners had scant options to address stiffness, aches, and myofascial pain. Only a few decades ago, there were no foam rollers or massage sticks, let alone the fancy gadgets designed to mobilize the stressed and strained muscles of endurance athletes.
Yet, while I don’t have the specific data, these self-mobility innovations have not reduced the number of manual therapy body workers and their collective workload.
Why? It may be that we as a society are more active — yet also stiff — as ever. Or that effective, pain-relieving tissue mobilization is a bit more complicated than a simple yet painful foam rolling session.
Specific to the lower leg, in this article I outline some advanced and specific tissue mobilization strategies to effectively improve soft tissue motion with less and less painful force.

Runners line up at the start of the 2018 Vibram Hong Kong 100k. Photo: iRunFar/Meghan Hicks
Thin Fascia Strategies
When treating issues of the foot and lower leg, it’s easy to focus entirely on either the most painful areas, or the dominant anterior and posterior foot and leg tissues for massage and stretching. Yet, our system is interconnected by layers of fascia, a very thin but strong connective tissue shrink-wrap that covers all of our bones and muscles.
There are important fascial lines that course not only on the top and bottom and front and back of the foot and leg, but also on the inside and outside. That may not seem like much tissue in these areas, but even this thin fascia on the inner and outer foot and ankle plays a crucial role in the mobility and function of the bigger groups of the plantar foot, calf, and outer shin.
Treating these areas with prolonged massage can improve tissue mobility in the whole system.
Tissue Play
My mentor, Gregg Johnson, PT, was a pioneer in bringing soft tissue mobilization techniques into the foray of physical therapy.
One unique concept he introduced was tissue play, the concept that individual tissues — muscle bellies, tendons, and their adjacent bones and fascia — should have free, independent movement. That lack of free movement between tissues (rather than a strain within a muscle or tendon, itself) is often the cause of myofascial pain.
Below is a cross-section of a left thigh, with the quadriceps group on the top and left, the adductors right, and the hamstring on the bottom. Each major group does a very different functional movement and needs muscle play for optimal, pain-free function.
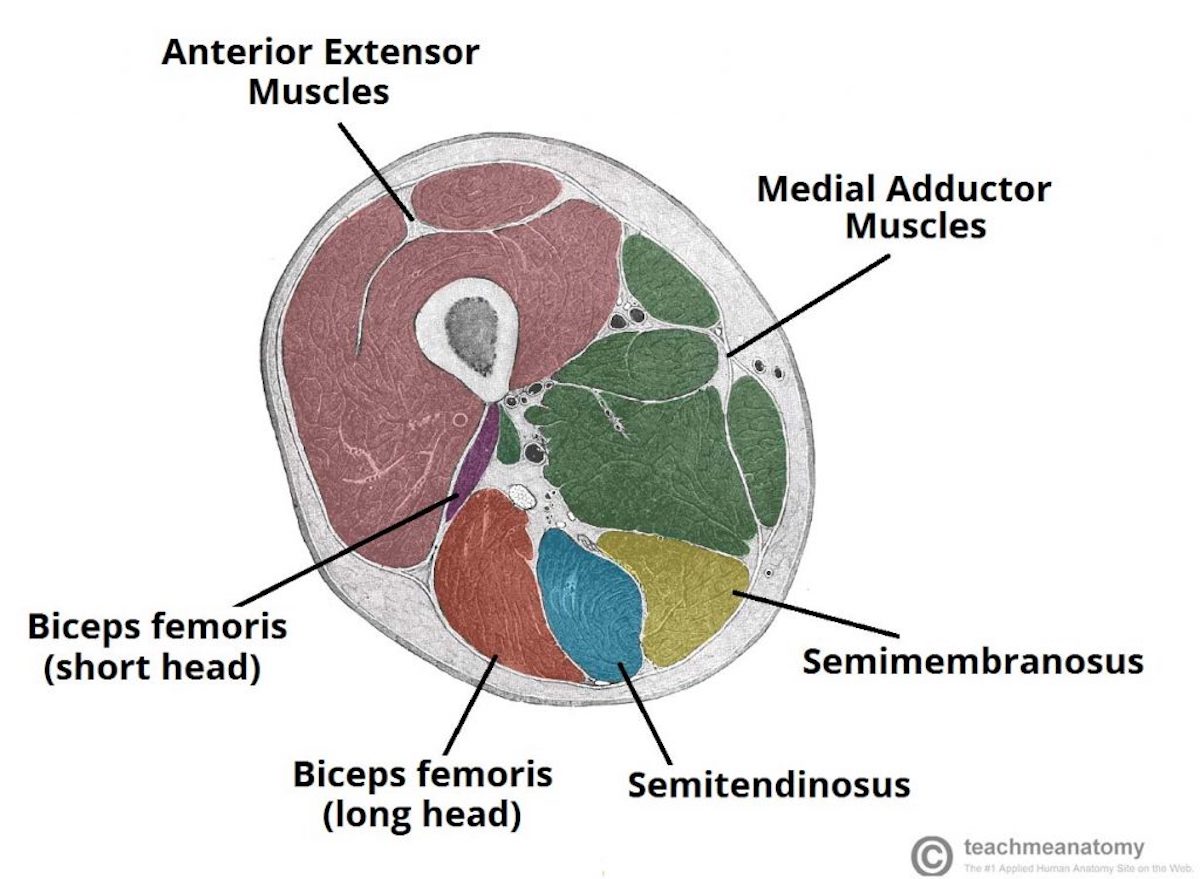
Image: Teachmeanatomy.info/lower-limb/muscles/thigh/hamstrings/
I think of tissue play, or a lack thereof, as the stickiness that can develop when cooking pasta. Often, cooked pasta noodles stick together. There is nothing wrong with the individual noodle; rather, chemical adhesions develop between the noodles, causing them to stick.
Even the individual muscles (or pasta noodles, in our example) within each compartment should have some degree of freedom from their neighbors.
A muscle play treatment helps restore this free, independent movement. It often involves freeing a specific tissue group from another adjacent group or from a bone. And while we can’t run a fork through it or cover it in oil like we can pasta, there are a couple of strategies to improve tissue play.
My favorite strategy involves applying perpendicular force to the tissue, while adding active or passive tissue movement.
Tissue Sliding
The classic soft tissue mobilization strategy involves a force application that compresses the tissue. But what if a tissue is stuck to an adjacent tissue, above or below it?
Think of our tissue like a layered sandwich. Each layer of our functional orthopedic sandwich — bread, lettuce, meat, and cheese — needs to be able to move independently of one another.
Straight compression, no matter how strong, is seldom an effective strategy to restore motion between one tissue layer and another.
Instead, a tissue sliding strategy is often more effective in restoring the motion and decreasing pain. This was another novel technique pioneered by Gregg Johnson to restore the independent motion of a specific tissue layer.
Tissue sliding is most important for the top layer of tissue, the superficial fascia, which runs beneath the skin, but above the muscles. Stiffness in this uppermost layer can result in tight, restrictive shrink wrapping of the muscles beneath it. Superficial fascial stiffness is often impervious to conventional muscle and joint stretching, and requires a tissue sliding strategy.
Tissue Distraction
Once again, conventional tissue mobility strategies involve compression. But if tissues are stuck together, another mobility strategy is distraction. Like lifting the top slice of bread off the sandwich, this involves a force application that pulls one layer of tissue away from the layers beneath it.
Cupping is the most common strategy to distract tissue. It involves a process of creating a negative pressure vacuum within the cup that suctions the tissue beneath it upward and away from the lower layers. Classic Eastern medicine cupping involves the use of a flame to create the vacuum, while modern cupping sets use a small pump to create a suction force.
Cupping is an effective distraction technique, but aggressive cupping — applying high vacuum pressures — can break small blood vessels and cause the characteristic and unsightly circular bruising often seen on the bodies of athletes.
A safer and arguably more effective distraction strategy is the use of a small plunger! While it may seem unsavory, having a small and dedicated manual therapy plunger in your arsenal is a great and less painful tissue mobility strategy, especially in areas where layers of tissue are tightly compressed along a bone.
Conclusion
Consider these advanced and alternative tissue mobilization strategies to help relieve lower leg pain and improve functional mobility. Also keep in mind that these strategies can be used with care in other parts of the body.
[Author’s Disclaimer: These soft tissue mobility strategies are not intended to cure any specific injury. They are for educational purposes only. It is recommended that you seek the opinion of a skilled professional before engaging in these techniques, and to ensure you are using safe and effective techniques.]
Call for Comments
- What therapeutic strategies have worked for you in decreasing lower leg pain? Foam rolling? Sauna? Something in this article?
- Have there been any nagging pains for you that aren’t necessarily injuries, but keep you from reaching your full running potential?

Hillary Allen letting her legs rest at the finish of the 2016 Transvulcania Ultramarathon. Photo: iRunFar/Meghan Hicks
