Stress fractures and other bone injuries, what are called bone stress injuries (BSI), occur commonly in long-distance runners. Desiree Linden, Tyler Pennel, Emily Infelt, Emma Coburn, Ryan Vail, Kara Goucher, and Mario Fraioli, just to name a few, have all sustained stress fractures and made them publicly known. The reasons we are hearing more about stress fractures may be due to a combination of an improved ability to diagnose them with magnetic resonance imaging (MRI), increased acceptance of athletes bringing these injuries to public attention, and because there are simply more people running.

Figure 1. Desiree Linden finishing second at the 2016 U.S. Olympic Trials Marathon, four years after a stress fracture. Image: Trackinfo
Do we runners think about the health of our bones? Though about 90% of our peak bone mass is achieved by age 18 in females and 20 in males, our bones are constantly remodeling and getting less and more resistant to fracture depending on what we eat, how much we weigh, the medications we take, and the amount and type of weight-bearing activities we do. A BSI can end a running season or career, especially if you keep running on it. It’s in your best interest to prevent and identify a BSI early if one does occur.
In this article, we provide a basic overview of BSIs including their epidemiology, risk factors, and locations. We also present emergent research data on bone health in the adult ultramarathon population. We interview Keely Henninger, Paul Terranova, and Craig Thornley about their recent fractures. Finally, we interview bone-health expert Dr. Emily Kraus.
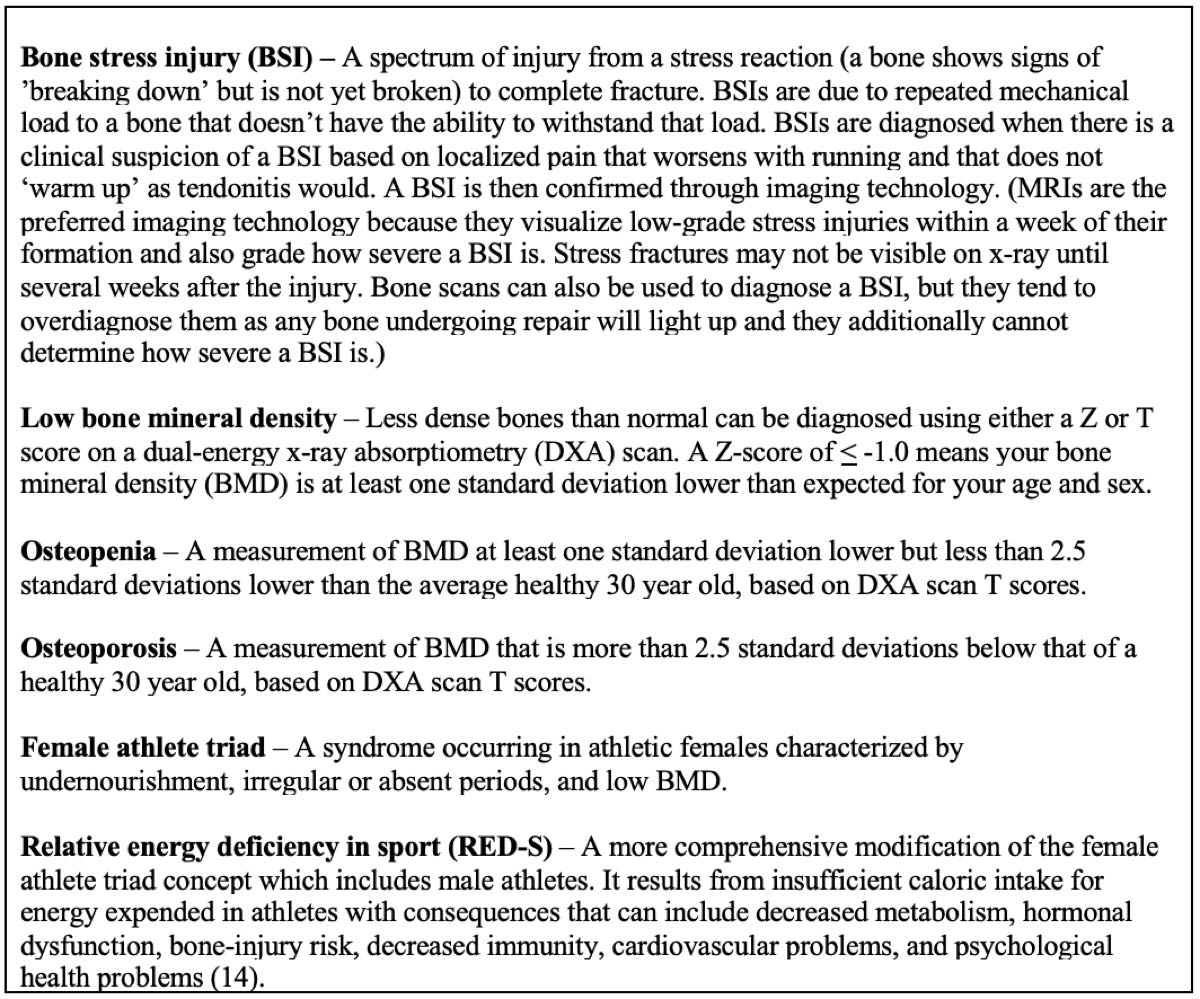
Figure 2. Key words and definitions that will help you better understand bone health in general and this article specifically. Image: Tracy Høeg
Bone Stress Injuries in Runners
One out of five collegiate runners is statistically predicted to have a BSI each year (10). Females have been previously found to be at higher risk (4), but recent work (10) suggests BSIs may be nearly as common in young men, with 27% of male college athletes sustaining a stress fracture over a two-year period. Stress fractures have been estimated to account for 20% of all musculoskeletal injuries in young-adult, competitive track-and-field athletes in one study (2) and 10% of all overuse running injuries in another study (13).
BSI incidence in adult ultrarunners was only studied for the first time in 2018, so we are just beginning to learn about it–and we’ll talk about it shortly in this article. However, if the incidence in competitive older adults is similar, that would make BSIs of the top two running injuries. Achilles tendonitis for example, has an incidence of seven to nine percent per year in current runners (11).
There are two types of bone tissues, cortical tissue which is hard and generally on the outside of a bone and trabecular tissue which is spongy and often on the inside of a bone. Typical trabecular-rich bones (think broad bones) that can fracture in runners include the head or neck of the femur, pelvis, sacrum, and the spine. Cortical-rich bones (think long bones) include the shaft of the femur, the tibia, fibula, and bones of the foot and heel. Half of BSIs in long-distance runners occur in the tibia, with the majority of other BSIs occurring in the femur, fibula, calcaneus (heel), metatarsals, and tarsals (foot bones) (26). Athletes with BSI at trabecular-rich sites such as the top of the femur, pelvis, sacrum, or spine should have their BMD assessed with a dual-energy x-ray absorptiometry (DXA) scan as they are more likely to have low BMD (15).
Figure 3 below demonstrates how BSIs progress. In this case, the tibia due to the progression of ‘shin splints’ goes from Grade 0/normal, to Grade 1 with swelling of the outside of the bone (periosteal edema), to grades 2 and 3 with swelling in the bone marrow, and to a Grade 4b fracture. To be clear, BSIs are expected to progress if the impact/stress and bone health remain the same.
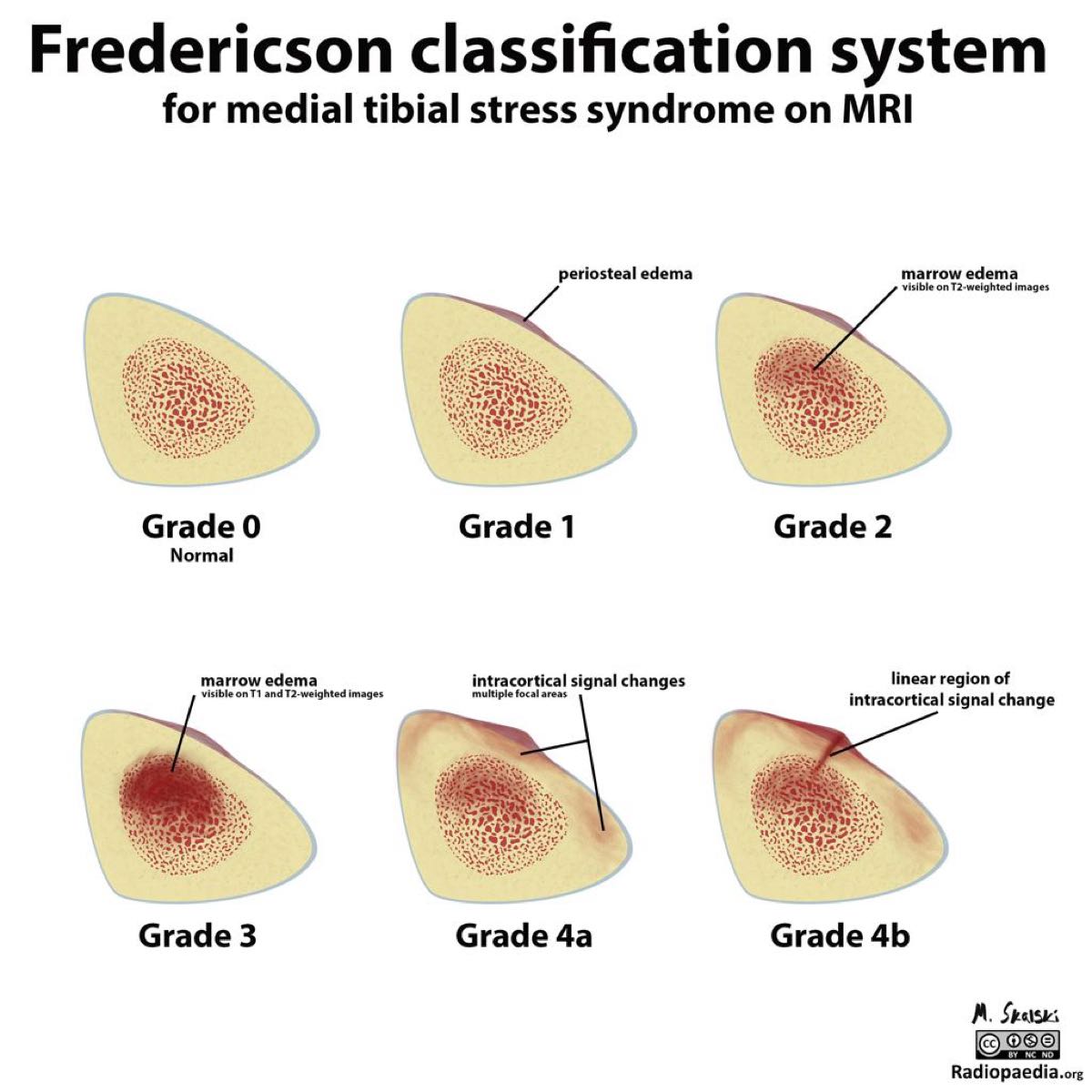
Figure 3. ‘Shin splints’ (Grade 1) can progress from a mild bone injury to a stress fracture or abnormality on x-ray (grades 3 and 4). Image: Fredericson M, Bergman AG, Hoffman KL et al (4)
The BSI grade is important because it can be used to estimate the amount of time off from running needed to heal the injury, as shown in Figure 4. BSI grades can be determined on MRI by your doctor possibly with the help of a radiologist.
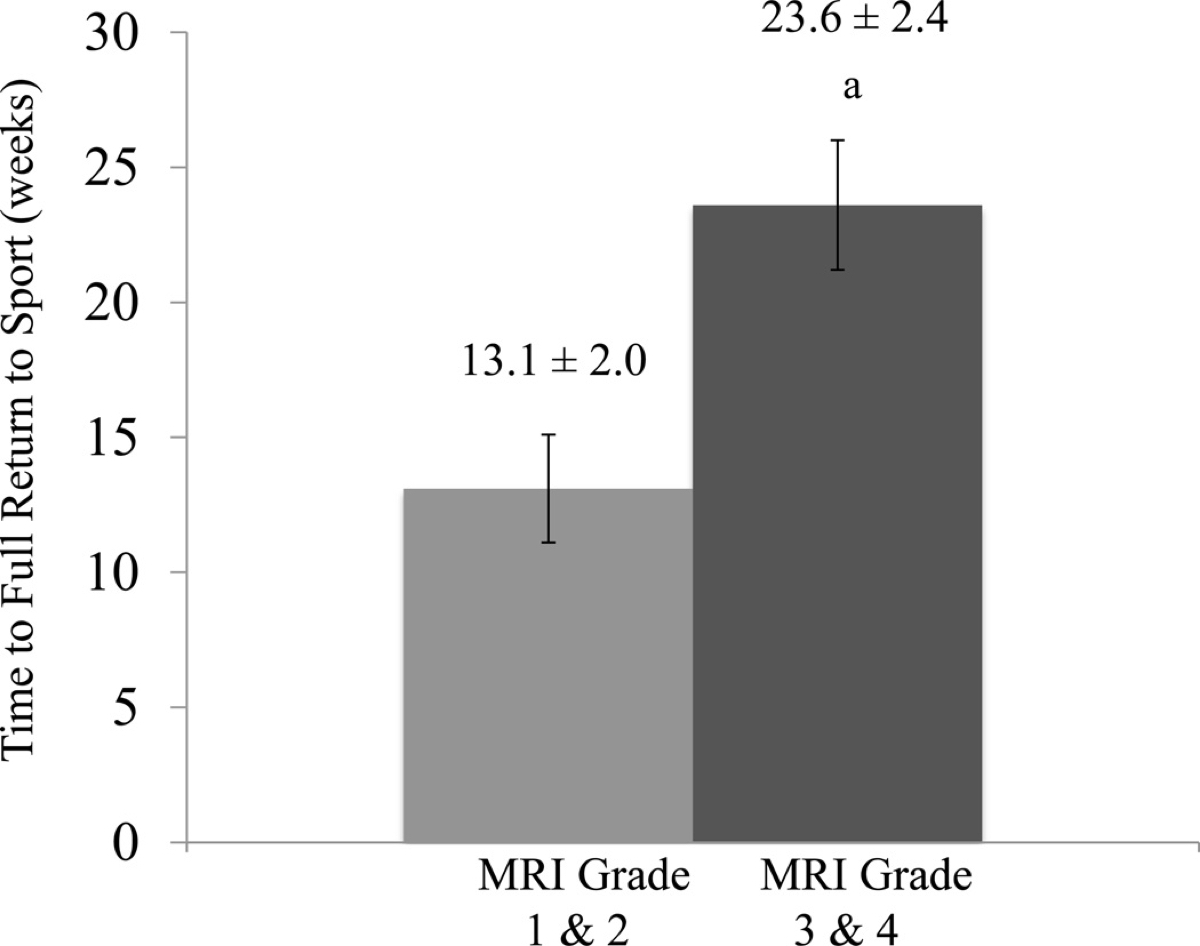
Figure 4. The time off required before returning to athletic participation for BSIs of different grades on MRI. Image: Nattiv A, Kennedy G, Barrack MT, et al (15)
As you can see, catching a BSI early is important. Sports-medicine physicians are ordering MRIs more often when they suspect a BSI to prevent the progression to a more serious injury.
Bone Stress Injury Risk Factors and Causes
In very simple terms, BSIs occur when the force applied to a bone supersedes its strength. One can develop a BSI due to either extrinsic factors (the load applied to the bone) or intrinsic factors (the strength of the bone). See Figure 5 for more.

Figure 5. The extrinsic and intrinsic factors that can lead to bone strain and cause a BSI. Image: Warden, Davis & Fredericson (26)
Extrinsic Bone Stress Injury Risk Factors
Extrinsic BSI risk factors that have been identified include running mileage (7), failure to take rest/recovery periods (13), shoes which are less shock-absorbent (6), caffeine consumption, alcohol consumption, and cigarette smoking (13). Additional extrinsic factors such as failure to change out shoes, running on harder surfaces, and increased training intensity all make intuitive sense as risk factors but do not appear to have yet been studied.
Intrinsic Bone Stress Injury Risk Factors
Intrinsic factors include nutritional status. Vitamin D and calcium status appear to have a dramatic effect on risk, at least in females. One blinded, randomized controlled trial showed that female Navy recruits who received vitamin D and calcium supplementation were 20% less likely to suffer BSIs (27).
One systematic review of stress-fracture risk (24) identified the largest risk reduction in females was achieved with consumption of 1,500 milligrams of dietary or supplemental calcium daily. The study (17) that identified this risk reduction from calcium intake was of 125 female, competitive distance runners who received annual DXA scans. They found that higher intake of calcium, skim milk, and dairy products were associated with lower rates of stress fracture. Each additional cup of skim milk consumed per day was associated with a 62% reduction in stress-fracture incidence and a high-dairy, low-fat intake was associated with a 68% reduction in incidence. Higher intakes of skim milk, dairy foods, calcium, animal protein, and potassium were associated with significant increases in whole‐body bone mineral density (BMD). Higher intakes of calcium, vitamin D, skim milk, dairy foods, potassium, and a dietary pattern of high dairy and low fat were associated with significant gains in hip BMD.

Figure 6. Milk is surprisingly effective for decreasing your risk of stress fracture. Image: Stefan Kühn
A number of medical conditions can influence bone health, including thyroid dysfunction, anemia, and decreased nutrient absorption from conditions such as gluten sensitivity, inflammatory bowel disease, and celiac disease (26).
Medications implicated in decreasing BMD (8) include:
- Antacids with aluminum
- Anti-seizure medications such as phenytoin
- Aromatase inhibitors (such as anastrazole)
- Chemotherapy
- Glucocorticoids (such as prednisone and cortisone)
- Gonadotropin-releasing hormone
- Heparin (anti-coagulant)
- Lithium
- Medroxyprogesterone acetate (Depo-Provera)
- Proton pump inhibitors
- Selective serotonin uptake inhibitors
- Tamoxifen
- Thiazolidinediones
- Thyroid medications in excess
In both men and women, insufficient fueling, participation in ‘leanness sports’ such as running, low body-mass index, low BMD, and BSI history are all risk factors (13, 10). Late menarche (15 years of age or older) (23) and irregular or absent periods (18) are risk factors for females and low testosterone may be a risk factor for males, though the latter has not yet been studied to my knowledge. The term ‘female athlete triad’ has largely been replaced in the sports-research community with the male and female-inclusive ‘relative energy deficiency in sport’ term, which is a syndrome of serious health problems that can result from inadequate nourishment to support the amount of physical activity undertaken. Male runners have about a six-fold increased risk of low BMD compared to their athletic but non-running peers (22). Female runners have about a five-fold increased BSI risk if they have low BMD (1).
But Running is a Weight-Bearing Sport, So Why Are Our Bones Breaking?
Yes, running is a weight-bearing activity, which is recommended to increase BMD, but clearly it does not prevent all BSIs. While running may tend to normalize lower-extremity BMD for age, it may not provide the bone strength needed for faster running, increased mileage, or new running surfaces.
The most effective cross-training exercises for increasing BMD (3):
- are dynamic not static;
- achieve adequate strain intensity;
- consist of discrete, intermittent bouts;
- include variable loading patterns; and
- are supported by optimal nutrition.
It is best if exercise involves loading in discrete bouts with recovery in between. Exercise should be of high magnitudes and/or rates, such as jumping for the lower body and racquet sports for the upper body (12).
Sports such as soccer, basketball, tennis, volleyball, and other high-impact, multiaxial-loading sports have been found to have more of an osteogenic effect than running in young male athletes (21). Research on the benefits of multiaxial-loading sports in adults hasn’t yet been done, but one could certainly extrapolate their benefits.
Bone Mineral Density Decreases After a Bone Stress Injury
Your BMD naturally decreases when you take time off from weight-bearing sports as well as when you convert from weight-bearing to non-weight-bearing sports such as cycling, swimming, and the elliptical. With just two weeks of non-weight bearing, a person can lose one to three percent of their BMD (20). If you have a BSI and take time off to to recover, you are expected to lose BMD, so your return to weight-bearing exercises should be extra gradual.
Bone Health in the Adult Ultrarunning Population
As previously discussed, bone health in collegiate runners has been well-researched, but until last year no research had been conducted specifically on adult ultramarathon runners. At the 2018 Western States 100, myself and Drs. Emily Kraus, Michael Fredericson, Marko Bodor, Emily Miller, and Kristin Sainani sought to learn about bone health in this population.
Kraus summarizes, “We enrolled 61 (20 female, 41 male) ultramarathoners racing the 2018 Western States 100. Each runner completed an online questionnaire looking at dietary habits (history of disordered eating/eating disorder), BSI history, and menstrual-dysfunction history in women. We also looked at BMD using DXA scans.” Adding one more detail (9), the mean age of our participants was 45.5 years.
Bone Mineral Density in Adult Ultrarunners
Twenty-one percent of females and 33% of males had low BMD for their age (Z score ≤ -1.0). See Figure 7 for more.

Figure 7. BMD in 2018 Western States runners. A Z score of -1 indicates the runner was a least one standard deviation below the mean in their age group, which is a sign of decreased BMD. A Z score of -2 is two standard deviations from the mean for the age group and represents more profound BMD decrease. Image: Kraus E, Høeg TB, Sainani K, Bodor M, Miller E, Weiss M, Fredericson, M (9)
The areas of decreased BMD in our ultramarathon population were as follows:
Males with Z scores < -1:
- Total hip: 12-14%
- Femoral neck: 5-6%
- Lumbar spine: 29.3%-33.3%
Females with Z scores < -1:
- Total hip: 0%
- Femoral neck: 5-6%
- Lumbar spine: 21-23%
The distribution of decreased BMD makes sense as there is more load through the hip while running than through the spine.
Compare this with collegiate runners where 10 to 11% of female runners have low BMD (Z score ≤ -1.0) (16) and 21.6% of adolescent long-distance runner males have low BMD (Z score ≤ -1.0) (1). That is, the males in our study had a higher prevalence of low BMD than adolescent or collegiate runners as well as a higher prevalence of low BMD than the female ultrarunners in our study.
Prior Bone Stress Injury in Adult Ultrarunners
As shown in Figure 8, 42% of females and 30% of males reported one or more prior BSI. The fact that a higher percentage of females reported a prior BSI than males is interesting and not consistent with the BMD data. However, this could suggest that despite having lower BMD, males still tend to have ‘enough’ to withstand the load applied during running.
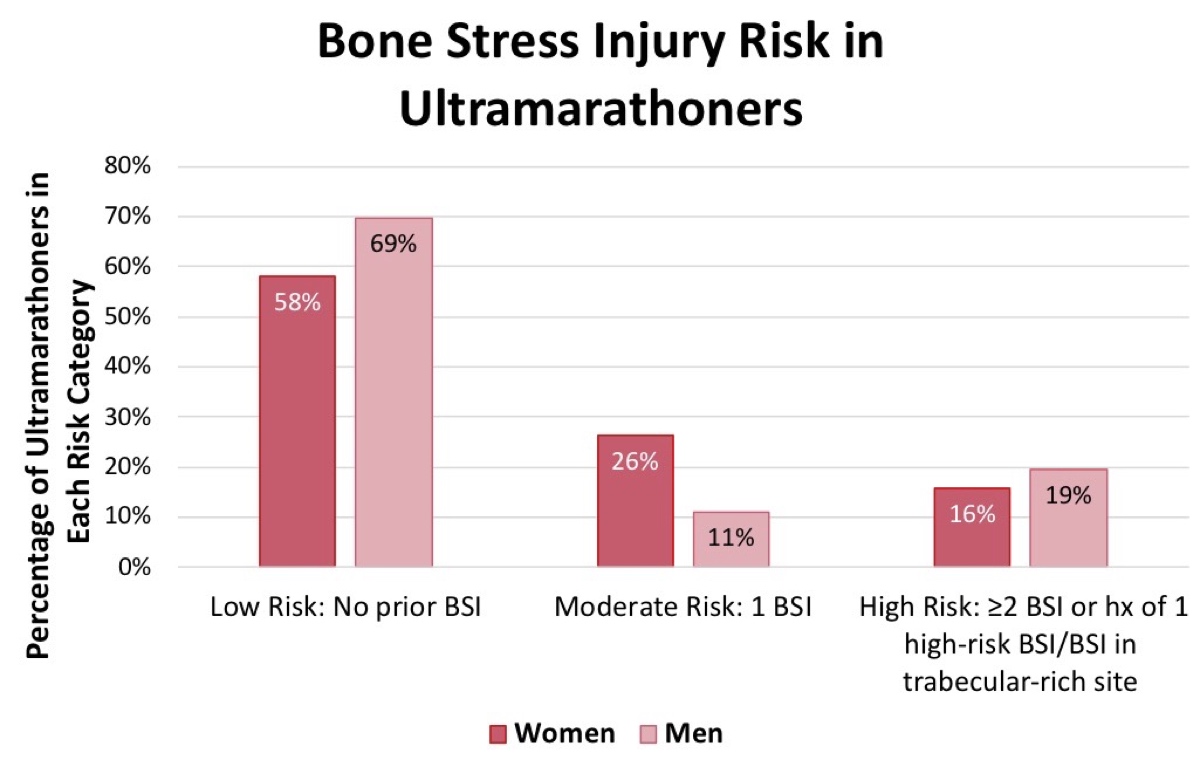
Figure 8. The number and types of BSIs in 2018 Western States runners. As discussed, bone has two components, cortical and trabecular, and BSIs in trabecular-rich sites are considered higher risk for BSI recurrence. Image: Kraus E, Høeg TB, Sainani K, Bodor M, Miller E, Weiss M, Fredericson, M (9)
Bone Stress Injury Risk Factors in Adult Ultrarunners
Some additional findings (9) were that 52.8% of males and 57.9% of females were at moderate or high risk for low energy availability (behavior consistent with inadequate calorie intake for a participant’s level of physical activity based on our questionnaire) and nine percent of runners had diagnosable eating disorders. Twenty-two-and-a-half percent of females and 0% of males were underweight. Among women, 42% reported a late start of their menses (age 15 or later) and 47% reported irregular periods.
Study Plans for the 2019 Western States 100
While exercise has been found to account for 30% of BMD variability (25), genetics appears to account for even more variation at 50 to 85% depending upon anatomical location (19). At the 2019 Western States, our research group will do genetic testing and pre-race bloodwork looking at ferritin, vitamin D, estradiol, and testosterone on participating runners. We will once again perform DXA scans and obtain health and lifestyle information on all study participants. The 2019 study will allow us to investigate the relationship between bone health and known genetic risk factors, hormones, ferritin, and vitamin D levels in adult ultrarunners.
Case Studies of Broken Bones in Adult Ultrarunners
Case #1: The Author’s Multiple Stress Fractures
When I was 22 years old and in medical school, I logged around 80 miles a week. I grew up playing soccer and basketball, so running had always felt relatively easy and I hadn’t had a running injury. On a cold winter night in Wisconsin, I was five miles from home on a run when I experienced sudden, excruciating pain in my left groin. I could not run one step further and had to hobble home.
It took months of suffering through pain with walking–I couldn’t run–and multiple health-care practitioners to properly diagnose my injury as a femoral neck stress fracture, which was at that time apparent on x-ray. After six months of swimming and the elliptical, I gradually restarted running. It was great at first, but then my shin, foot, and everything in my legs hurt. I will still running relatively low mileage compared to what I had run before the fracture. I had a DXA scan and a bone scan done. (Bone scans were previously used for evaluating BSIs before MRIs came into fashion.) The bone scan showed small stress fractures all over the place and the DXA scan brought even worse news that I had osteoporosis in my spine and osteopenia in my hip and arm.
It took a while and actually being admitted to the hospital with malabsorption causing profound anemia to discover what had led to my poor bone health. Here was my quintuple whammy of BSI risk factors:
- Low body-mass index (just under 17.5 at the time);
- Use of Depo-Provera birth control;
- Six years of amenorrhea, which physicians either attributed to ovarian cysts or Depo-Provera;
- Celiac disease causing the malabsorption and anemia; and
- Long-term use of a proton pump inhibitor for my gastro-intestinal issues.
Shortly thereafter, I started my clinical rotations in medical school and had a lot less time for running. I cut back on my mileage by about 50% and also gained 15 pounds, though I did eventually lose that weight a few years later. I also made changes to my diet and medications. I am happy to report that I have not had a BSI since, I am now 39, and I have logged many 100-plus-mile weeks.
Case #2: Keely Henninger’s Pelvic Stress Fracture
Leading up to Keely Henninger’s stress fracture in March of 2019, she’d been dealing with a rough period. She had a nagging right hip-adductor injury. She had decreased motivation, decreased appetite, difficulty sleeping, and mood changes. Also, her bloodwork showed her vitamin D below normal and ferritin at the low end of normal.
She began experiencing posterior hip pain on a run and quickly knew this was the type of injury she could not run through. After working with several health-care practitioners, she got an x-ray and MRI about one week after the pain started. The MRI showed a pelvic stress fracture as well as a hip labral tear on the same side.
She was given crutches to use until normal walking was pain free. She took two weeks entirely off of exercise. “I did not even go to yoga,” she states. “It was just what I needed.” She felt like a new person after those two weeks and gradually started to increase her cross training, first with cycling and then swimming. In total, she took 10 weeks off running and is currently, as of June of 2019, rebuilding her mileage and supplementing with cross training.
Keely has an interesting health history. A few years ago, far prior to this injury, she was found to have elevated testosterone and below-normal ferritin. She was eventually diagnosed with polycystic ovarian syndrome (PCOS), which is known to cause irregular periods as well as insulin resistance similar to that seen in diabetes. She made drastic changes in her diet, decreasing her consumption of processed carbohydrates and increasing her red-meat consumption. Her lab values returned to within normal, but over the past year she said her ferritin was drifting down, she had below-normal vitamin D, and she was less careful about watching her diet.
She believes this and her continuing to train through niggles and not taking a significant period of time off this past year led to the injury. She states, “In trail and ultrarunning, there is no off season. In Europe, they take the winter off to ski and gain 10 pounds. Maybe we should do this in the United States.” Finally, she discussed that she for many years had irregular periods. While this was likely related to her PCOS, she stated, “I want you to put this in the article: Women sometimes consider it a badge of honor to not get their period. Like that means they are working really hard. But it is not right and not healthy. Women who don’t get their period regularly should have it looked into. I think more women are supporting their female running colleagues in this, which is awesome.”
Case #3: Paul Terranova’s Femoral Shaft Stress Fracture
In late 2017, Paul Terranova strained his right hamstring, high in the muscle, while catching his toe on a run–a common occurrence for trail runners. The injury was one he was able to manage and train through. But in May of 2018, on what he described as “a typical three-hour, 16-mile training run” while in an intense training period for the Western States 100, he felt the sudden onset of a totally different kind of pain, around the right IT band and lateral knee. For almost a month he sought the help of multiple health-care practitioners while only doing non-weight-bearing exercise, and everyone’s work was focused on diagnosing and treating the IT band and knee. He even got an MRI in mid-June, but only of the right knee and lower leg, which were clear. He was also able to run five miles without pain around that time, so he flew from home to the race starting line in California. There, a doctor friend watched him run and advised him not to start the race. (This video shows what his running looked like then.)

Figure 10. Paul Terranova on his way to winning the 2019 Cruel Jewel 100 Mile after recovering from a femoral shaft stress fracture. Image: Kristopher Cargile
He didn’t run the race, and instead sought the assistance of another health-care practitioner who ordered multiple tests, including a bone scan. Paul recounts that doctor saying the bone scan “lit up my mid-right femur like Christmas.” An MRI also diagnosed the femoral shaft stress fracture as well as a chronic tear of the hamstring where it attaches in the pelvis. Electromyography (a nerve-function test) also identified a problem with the nerve located at the L5 vertebrae in his back.
iRunFar: Once they new it was a stress fracture, did they grade it or what did they base your time off of running on?
Paul Terranova: In terms of my recovery, my doctor estimated about 12 weeks:
- three to four weeks on crutches and just swimming, stationary bike, and elliptical machine to minimize risk of completing the fracture;
- three to four weeks of walking/hiking with poles/Alter-G treadmill sessions at reduced bodyweight; and
- three to four weeks of gradually reintroducing ground running at 100% bodyweight.
I had three check-ups with my doctor and they did x-rays for the first two and everything was progressing well. I also used a prescribed Exogen Ultrasound Bone Healing System during this period and into early 2019. [Author’s Note: This is a bone stimulator.]

Figure 11. Paul Terranova’s bone scan with the shaft of his fractured right femur lighting up. Image courtesy of Paul Terranova.
iRunFar: And what sort of work-up did they do in terms of causes? Did you have a DXA scan? Bloodwork drawn? Do you take any medications or have any health or family history that could have contributed to this? Was this your first BSI?
Terranova: I did not have a DXA scan. I had a full physical and bloodwork done with my regular sports doctor in July of 2018, and nothing was identified as abnormal. Specifically, vitamin D, calcium, ferritin, and testosterone were all normal. This was my first BSI and I do not have a health or family history that would contribute to it.
iRunFar: Are you back to your pre-injury running mileage and racing?
Terranova: Yes. My coach was awesome about gradually getting me back to running, patiently allowing my muscular strength to catch up to my cardiovascular fitness, and then we added intensity and then volume. I raced for the first time again in September, a 35-kilometer race. Since then, I’ve done three 100 milers.

Figure 12. X-ray of Paul’s femur showing a linear fracture, circled in blue. Image courtesy of Paul Terranova.
Thoughts on Muscle Imbalance/Injury as Possibly Predisposing to a Bone Stress Injury
Keely’s pelvic fracture combined with a preceding hip-adductor injury and Paul’s femoral shaft fracture combined with a preceding hamstring injury made me wonder if the muscle tightness caused by muscle injury actually pulled on the bone to such a degree that a fracture occurred. Please see the origin of the highlighted adductor and short head of the hamstring highlighted in figures 13 and 14.
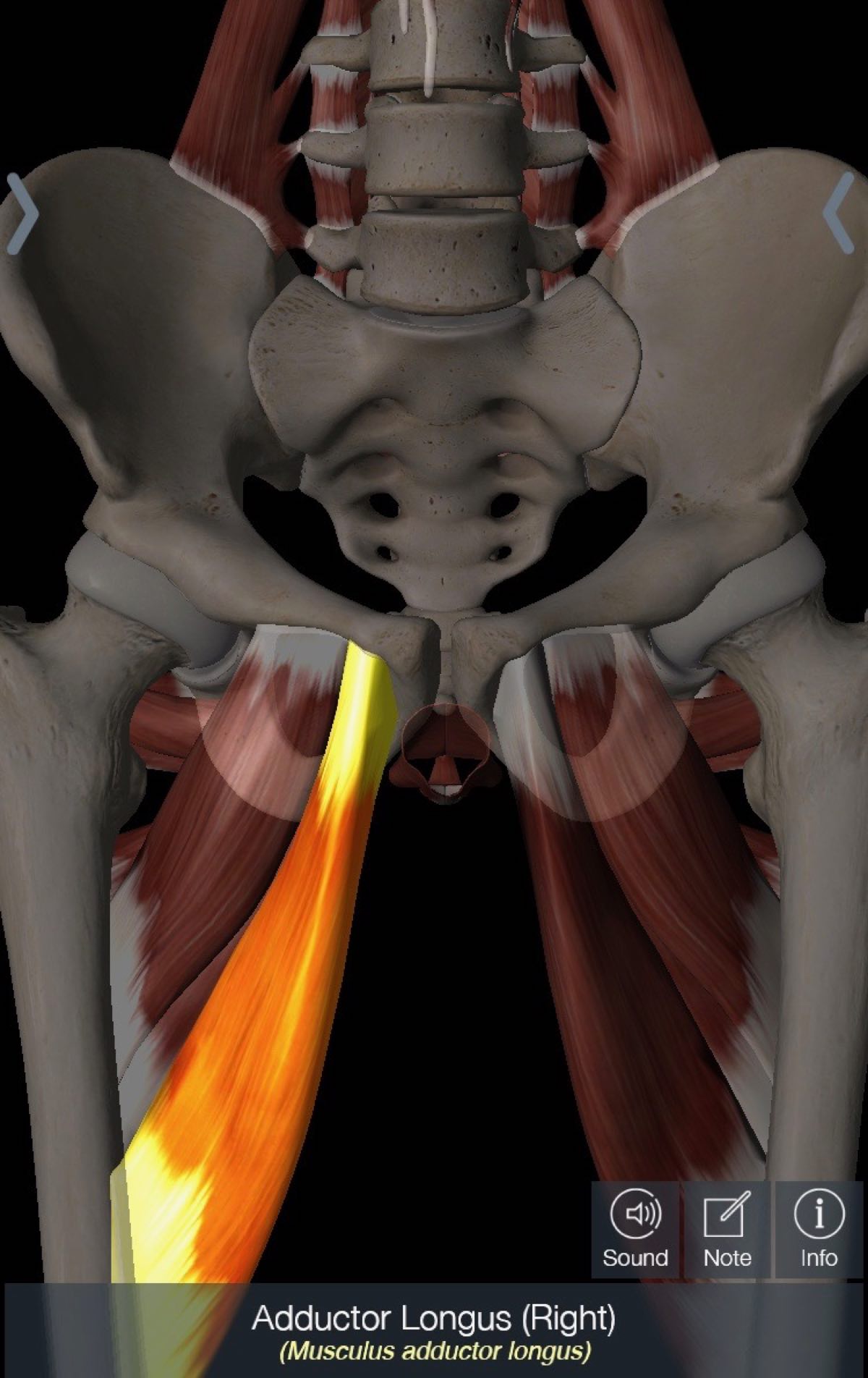
Figure 13. The adductor longus muscle, which Keely had strained prior to her BSI, with its origin on the pelvis. The muscle originates on the anterior part of the pelvis and her injury was in the back, but I wonder if the tight muscle led to an imbalance that caused the fracture? Image: Tracy Høeg
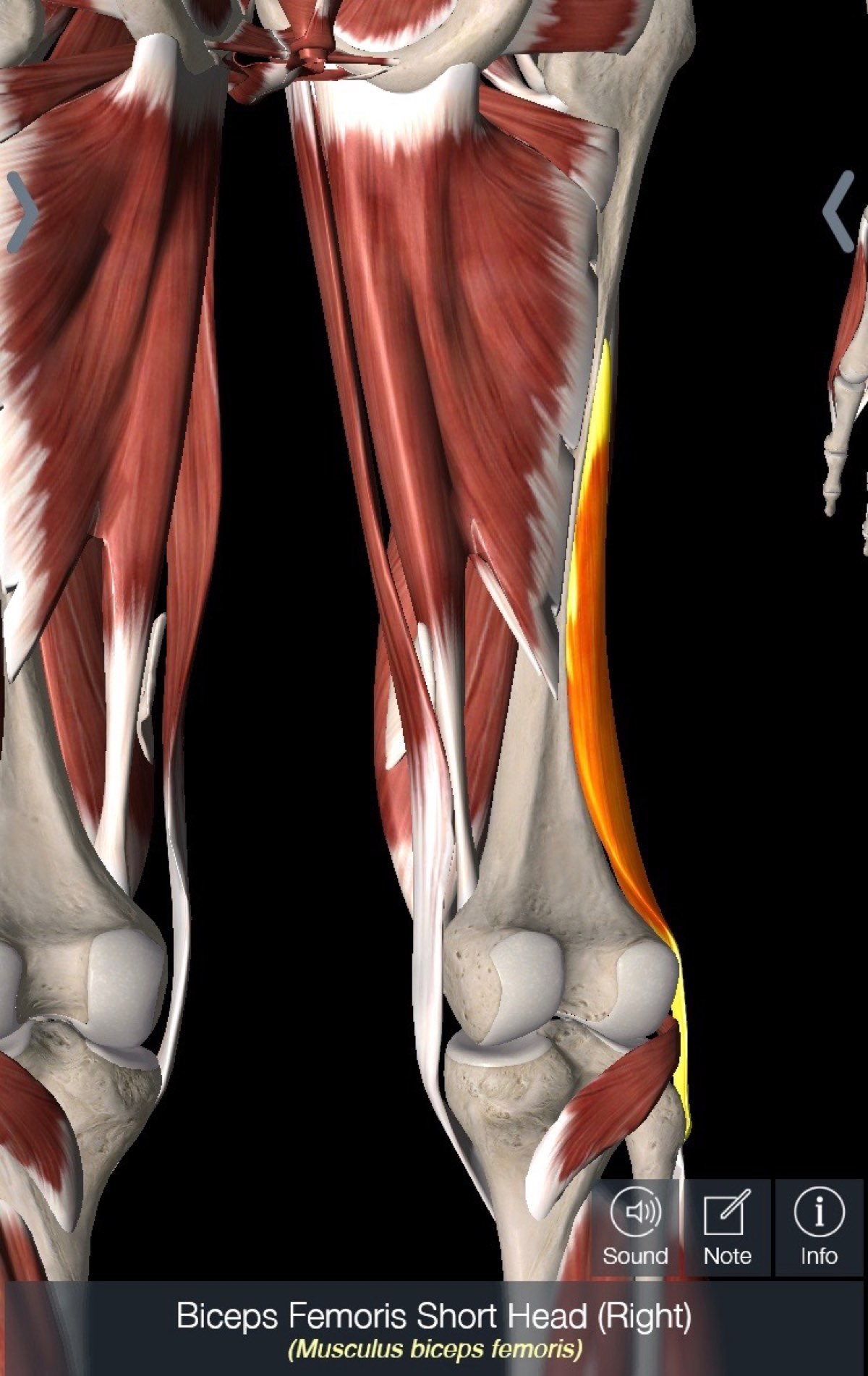
Figure 14. The biceps femoris (hamstring muscle), which Paul had strained prior to his BSI, with its origin on the posterior mid-shaft of the femur, which is exactly where his BSI was. Image: Tracy Høeg
Case # 4: Craig Thornley’s Metatarsal Avulsion Fracture
Craig Thornley was recently doing speedwork on a track when he sustained a fracture to his fifth metatarsal. Though this is not a BSI resulting from repetitive stress and instead a sudden injury, it’s another example of the kind of bone injuries ultrarunners can experience.
iRunFar: Craig, I am sorry about your injury. Can you tell me about what happened?
Craig Thornley: I was doing speedwork when I had sudden onset of pain in the outside of my left foot. I had never had pain here before and I knew it was serious right away because my foot swelled up immediately and I had trouble walking. The next day, I went to see my chiropractor who wouldn’t touch my foot before I got an x-ray.

Figure 16. Craig’s x-ray, with the avulsion fracture of the fifth metatarsal circled in red. Image courtesy of Craig Thornley.
Interview with Dr. Emily Kraus
Emily Kraus, MD, is a clinical Assistant Professor at Stanford Children’s Orthopedic and Sports Medicine Center and a self-described ”enthusiast of running, the outdoors, sports medicine, bone health, injury prevention, and the female athlete.”
iRunFar: Emily, I know that DXA scans are generally only recommended for women over 65 and certain other populations that are high risk for osteoporosis, but based on the preliminary results of our study of ultramarathon runners, would you recommend DXA scan screening for ultramarathon runners with decreased BMD? If so, all or just ones with certain risk factors?
Emily Kraus: Just so we’re all on the same page, it’s important to discuss the impact low energy availability (inadequate energy/caloric intake for the level of exercise) can have on bone health. We have defined this in females as the female athlete triad, which includes menstrual irregularities, low energy availability, and impaired bone health. We are finding a similar phenomenon in males with the main difference being alterations in other sex hormones.
Regarding the decision to screen all or some ultramarathoners using DXA scan, I think it’s too soon to make any type of formal recommendation, given the still-limited research in this athlete subgroup. I agree with you that male and female ultramarathoners who present with certain risk factors should discuss a DXA scan with a sports-medicine physician.
Based on the latest guidelines by The International Society for Clinical Densitometry, a DXA scan is indicated for women younger than 65 years and men younger than 70 years if they have certain risk factors such as low body weight, prior BSI, high-risk medication use, and/or a disease or condition associated with bone loss.
It is also well-supported to perform DXAs on high-risk female athletes based on risk factors related to the female athlete triad. We’re still determining which risk factors carry the greatest weight in male ultramarathoners, which is one of the reasons we’re continuing the study this year.
iRunFar: Recently, I wrote an article on screening laboratory tests in runners and recommended against routine screening in otherwise healthy runners, with the exception of an iron panel in females. But would you recommend routine testing of vitamin D, estradiol, testosterone, or anything else in endurance runners? And what lab tests should a runner get if they have sustained a BSI?
Kraus: I agree with you. A blanket recommendation to screen all endurance runners without a clinical question–such as ‘why am I so fatigued despite adequate rest?’–is usually unnecessary. I do encourage screening labs if an athlete is considering supplementing with iron or vitamin D or if the athlete (male or female) is vegan or vegetarian and there may be question of inadequate iron intake.
For an athlete who sustained a BSI, I recommend tests for vitamin D and an iron panel. And if there is concern for menstrual dysfunction in females or other hormonal imbalances in males, I would consider additional hormonal work-up, but it depends on their age and the symptoms’ severity.
iRunFar: Do you have any specific guidelines you use for rehabilitation from a BSI and reloading the affected body part? Would you have an athlete progress through hopping and jumping activities and sports before they start running again? Or should this be done in general to promote good bone health?
Kraus: Rehabilitation from a BSI depends on the location and severity. Some high-risk sites require longer bouts of non-weight bearing. Once the bone is healed, it’s important to gradually re-introduce loading to the bone to avoid re-injury. It’s also often overlooked that some bone mass is lost after this period of non-weight bearing so there is a transient risk to other parts of the bone on that limb if volume is increased too quickly.
As part of the rehab course, I recommend getting into some good physical therapy to incorporate resistance training into the healing process. This is good practice during recovery and will also be valuable to continue once in regular training. Resistance exercises are an excellent stimulus to build bones! I would advise against any hopping/jumping activities until further along in the running progression.
iRunFar: Could you also comment on the role of ferritin in bone health? Iron deficiency is quite common in runners and I wonder if this might be an under-discussed cause of decreased BMD in long-distance runners.
Kraus: I do think there’s a relationship between iron deficiency and bone health. There’s a great article discussing the unexplored crossroads of iron deficiency and the female athlete triad. In the article, they discuss how low iron may throw off some of the hormonal axes, specifically growth hormone and thyroid function. I don’t think we can make any associations between iron deficiency being the cause of low BMD in distance runners, but I do think it’s an area that should be studied further.
iRunFar: Finally, could you share your impressions on our findings from the 2018 Western States 100 bone-health study? Were any of the results surprising to you?
Kraus: I was surprised to see the number of males with low BMD. It was also interesting that we found statistically significant associations with low BMD and BSI history in males.
In Summary
- A bone stress injury (BSI) is an overuse injury whereby the bone is loaded more than it can tolerate and that causes pain that increases with running and does not decrease after warming up (as a tendon injury does).
- BSIs are common in runners. New research is showing that decreased bone mineral density (BMD) and prior BSIs appear to be at least as common in the adult ultrarunner population as in the collegiate runner population.
- BSIs occur due to modifiable extrinsic and intrinsic risk factors related to training and health. Adequate caloric intake, calcium intake, vitamin D levels, and a regular menstrual cycle in women, in addition to participation in weight-bearing sports, are all important for your bone heath.
- Do not ignore BSI warning signs. If you have pain that does not warm up with running or increases, seek medical care. Identifying a BSI early may prevent a fracture and/or shorten your recovery time.
Call for Comments (from Meghan)
- Have you had a stress fracture or other bone stress injury?
- Can you share a little about your injury experience, from the injury onset and pain, risk factors you have, the diagnosis process, and how rehabilitation went?
References
- Barrack MT, Fredericson M, Tenforde AS, et al. Evidence of a cumulative effect for risk factors predicting low bone mass among male adolescent athletes. Br J Sports Med 2017;51:200–205.
- Bennell KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD. The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Am J Sports Med1996;24:211-7.
- Borer KT. Physical activity in the prevention and amelioration of osteoporosis in women: interaction of mechanical, hormonal and dietary factors. Sports Med. 2005;35:779-830.
- Brukner PD, Bennell KL. Stress fractures in runners. J Back Musculoskel Rehabil. 1995;5:341Y351.
- Fredericson M, Bergman AG, Hoffman KL et al. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995. 23 (4): 472-81.
- Gardner LI Jr, Dziados JE, Jones BH, et al. Prevention of lower extremity stress fractures: A controlled trial of a shock absorbent insole. Am J Public Health 1988;78:1563-1567.
- Gilchrist J, Jones BH, Sleet DA, Kimsey CD. CDC. Exercise-related injuries among women: Strategies for prevention from civilian and military studies. MMWR Recomm Rep 2000;49(RR-2):15-33.
- Goolsby MA, Boniquit N. Bone Health in Athletes. Sports Health. 2017 Mar-Apr;9(2):108–117. doi:10.1177/1941738116677732
- Kraus E, Høeg TB, Sainani K, Bodor M, Miller E, Weiss M, Fredericson, M. Identifying Risk Factors Associted with Bone Stress Injury in Ultramarathon Runners. Oral Presentation at the American Medical Society for Sports Medicine annual conference in February of 2019.
- KrausE, Tenforde AS, Nattiv A, et al. Bone stress injuries in male distance runners: higher modified Female Athlete Triad Cumulative Risk Assessment scores predict increased rates of injury. British Journal of Sports Medicine 2019;53:237-242.
- Maffulli N, Wong J, Almekinders LC. Types and epidemiology of tendinopathy. Clin Sports Med 2003;22:675–92
- Manske SL, Lorincz CR, Zernicke RF. Bone health: part 2, physical activity. Sports Health. 2009;1:341-346.
- McInnis KC and Ramey LN. High Risk Stress Fractures: Diagnosis and Management. PMR. 8 (2016). 5113-5124.
- MountjoyM, Sundgot-Borgen J, Burke L, et al. The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S). British Journal of Sports Medicine 2014;48:491-497.
- Nattiv A, Kennedy G, Barrack MT, et al. Correlation of MRI grading of bone stress injuries with clinical risk factors and return to play: a 5-year prospective study in collegiate track and field athletes. Am J Sports Med. 2013;41(8):1930–1941. doi:10.1177/0363546513490645
- Nattiv A, Loucks AB, Manore MM, et al. The American college of sports medicine position stand on the female athlete triad. Med Sci Sports Exerc 2007;39:1867–82.
- Nieves, J. W., Melsop, K. , Curtis, M. , Kelsey, J. L., Bachrach, L. K., Greendale, G. , Sowers, M. F. and Sainani, K. L. (2010), Nutritional Factors That Influence Change in Bone Density and Stress Fracture Risk Among Young Female Cross‐Country Runners. PM&R, 2: 740-750.
- Pegrum J, Crisp T, Padhiar N. Diagnosis and management of bone stress injuries of the lower limb in athletes. BMJ 2012;344: e2511.
- Ralston SH, Uitterlinden AG. Genetics of osteoporosis. Endocr Rev. 2010;31(5):629–662.
- Rittweger J, Simunic, Bilancio et al., “Bone loss in the lower leg during 35 days of bed rest is predominantly from the cortical compartment,” Bone, vol. 44, no. 4, pp. 612–618, 2009.
- Tenforde AS, Fredericson M. Influence of sports participation on bone health in the young athlete: a review of the literature. PM R. 2011;3(9):861–7.
- Tenforde et al. Low Bone Mineral Density in Male Athletes Is Associated With Bone Stress Injuries at Anatomic Sites With Greater Trabecular Composition. Am J Sports Med.2018 Jan;46(1):30-36.
- Tenforde AS, Sayres LC, McCurdy ML, Sainani KL, Fredericson M. Identifying sex-specific risk factors for stress fractures in adolescent runners. Med Sci Sports Exerc 2013;45: 1843-1851.
- Tenforde AS, Sayres LC, Sainani KL, Fredericson M. Evaluating the relationship of calcium and vitamin D in the prevention of stress fracture injuries in the young athlete: A review of the literature. PM R 2010;2:945-949.
- Valdimarsson Ö, Kristinsson J, Stefansson S, Valdimarsson S, Sigurdsson G. Lean mass and physical activity as predictors of bone mineral density in 16–20-year old women. J Intern Med. 1999;245(5):489–496.
- Warden, Davis & Fredericson. Management and Prevention of Bone Stress Injuries in Long Distance Runners. J Orthop Sports Phys Ther 2014;44(10):749-765. Epub 7 August 2014.
- Lappe J, Cullen D, Haynatzki G, Recker R, Ahlf R, Thompson K. Calcium and vitamin d supplementation decreases incidence of stress fractures in female navy recruits. J Bone Miner Res. 2008 May;23(5):741-9. doi: 10.1359/jbmr.080102.



