With this article, my goal is to provide an in-depth understanding of:
- What exercise-associated hyponatremia (EAH) is and why it occurs with exercise;
- Why overhydrating during exercise can be so dangerous;
- How to recognize EAH when it does occur;
- How EAH is best treated; and
- How EAH is best prevented (and why salt supplements are not necessarily a good prevention strategy).
As an iRunFar reader, I expect that most of you have some familiarity with the above concepts. I hope this article will not only provide more details about EAH for you, but also that you can teach others about EAH in your roles as coaches, fitness instructors, exercise physiologists, health-care workers, journalists, and more.
Definitions
Here are a few definitions to get us all speaking the same language.
Exercise-associated hyponatremia (EAH): A low blood plasma sodium level that develops during exercise. In most labs, this is defined as and Na+ (sodium) of less than 135 mEq/L. The normal Na+ range either during or outside of exercise is 135-145 mEq/L.
Arginine vasopressin (AVP)/antidiuretic hormone (ADH): Two names for the same hormone which is released from the pituitary gland in response to dehydration and increased sympathetic drive (the ‘fight-or-flight response,’ which occurs during exercise, stress, pain, and more). As examples, this hormone is known to be released in heart failure, respiratory failure, various cancers, and in muscle breakdown.
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH): When the hormone ADH is not released in response to dehydration, but instead in response to one of the stressors listed above. SIADH is believed to be the major physiologic occurrence, when coupled with drinking fluids, that predisposes humans to EAH.
Introduction
I was recently taking a class at our local gym and the instructor said numerous times, “Remember to keep drinking and finish your bottle by the end of class.” It was a 45-minute class. The notion that unlimited hydration is what all of us should strive for during exercise is so ingrained in the fitness world that I sometimes wonder if it can be unlearned. Maybe you, too, have been running a trail race and an aid-station volunteer offered you the seemingly helpful advice to “stay hydrated.” Maybe you are thirsty and that is what you need, but I hope when you have finished reading this article that you will see why this advice to “keep hydrating” can be so dangerous. Specifically, not only can athletes become ill from EAH, but deaths have occurred due to EAH in numerous sporting activities including but not limited to marathon running, military drills, hiking, and American football.
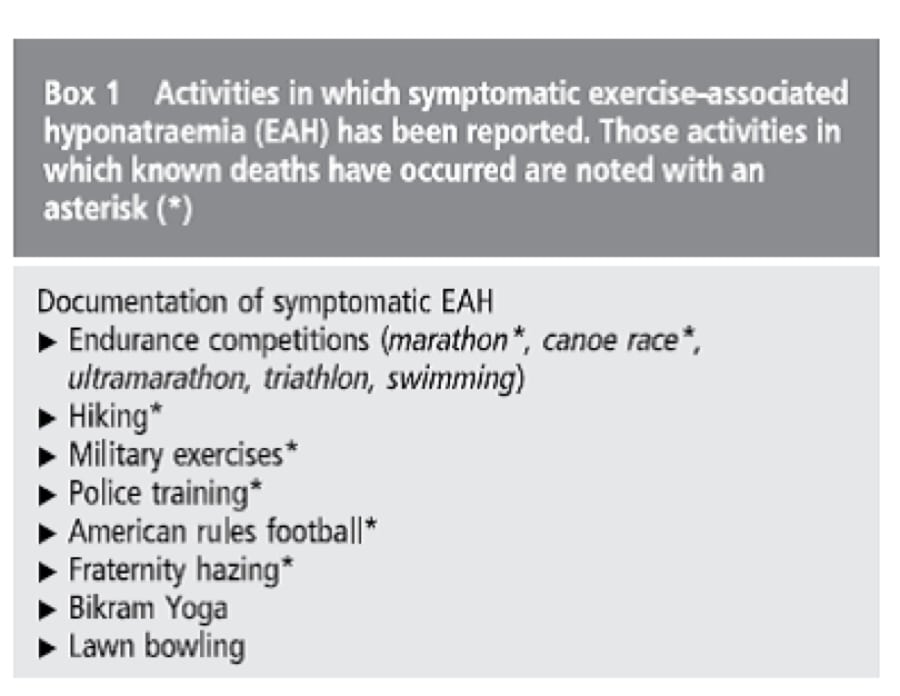
Figure 1. Activities where exercise-associated hyponatremia has occurred, including known deaths (Hew-Butler, 2017).
Historical Background
Cynthia Lucero, a previously healthy 28-year-old female, was running her second marathon, the 2002 Boston Marathon. She was the type of person who thoughtfully planned ahead. She had just completed her doctoral dissertation entitled “Effects of a Marathon Training Program on Family Members and Friends of Cancer Patients.” And that day, she was running to raise money for the Massachusetts Chapter of the Leukemia and Lymphoma Society.
Her race was going as planned. She had numerous friends watching her run and they reported that she drank copious amounts of Gatorade at every aid station, which were one mile apart. She looked strong at mile 20’s Heartbreak Hill, but then, just before mile 22, she started to lose her footing. She looked to be struggling so much that a friend jumped into the race to run alongside her. Cynthia said she felt “rubber legged” and then collapsed to the pavement (Smith, 2002).
An ambulance took her to Brigham and Women’s Hospital where she was found to be in a coma. A breathing tube was placed and she was given intravenous (IV) fluids (normal 0.9% saline, or a fluid-salt solution that is isotonic with human blood–in other words, it will not cause ‘pickling’ or swelling of human tissues) and her sodium level was found to be 113 mEq/L, far below the normal 135-145. She was found to have diffuse cerebral edema, or brain swelling, and elevated arginine vasopressin (AVP), consistent with EAH. Shortly thereafter, she was found to be braindead (Siegel, 2007). This was only the second death in the race’s long history.
And then, just six months later, in October of 2002, it happened again, in an eerily similar way. Hillary Bellamy was running the Marine Corps Marathon and, at mile 21, she felt so sick that she left the race course (Orton, 2006). She was transported by ambulance to the nearest hospital, still coherent, and was given IV fluids (again 0.9% saline). She then proceeded to go into a coma. Her sodium level was 123 and her AVP was elevated, consistent again with EAH, but a milder case. However, she too would go on to die of cerebral edema two days later (Siegel, 2007).
Numerous similar cases occurred in the 2004 and 2005 Boston and Marine Corps Marathons, where runners became comatose, developed seizures, or experienced other neurologic complications from EAH (Seigel, 2007).
However, now the treating physicians had figured something important out: they needed to treat these runners with a more concentrated sodium solution, in other words hypertonic (3% saline) IV fluids. Hypertonic fluid is a salt-fluid solution with higher tonicity/concentration than normal blood—it will cause pickling of human cells. Importantly, in this case, it will promptly reduce the brain swelling. By doing so, they stopped a potential scourge of deaths at these races (Siegel, 2007).
But let’s rewind a second, why were runners now getting this previously unknown entity of EAH in scores? Honestly, it should be said that, already in 1985, life-threatening cases of “water intoxication” were starting to crop up at the Comrades Marathon, including runners with seizures and hospitalizations. Fortunately, all survived. Then, in 1986, two physicians running 80- and 100-kilometer races respectively in Chicago, Illinois both developed EAH so severe that they required hospitalization (Frizzell, 1986). They had both been advised to drink 300-360 milliliters/10-12 fluid ounces every mile (at each aid station). They were treated at separate hospitals; one received hypertonic 3% saline and was discharged home the same day and the other received isotonic 0.9% saline and was semi-comatose for 36 hours and developed numerous complications before finally being discharged after five days (Frizzell, 1986).
By the end of 1986, a body of evidence (Noakes, 1985; Frizzell, 1986; Noakes & Speedy, 2006) showed that:
- EAH in runners was related to excessive fluid consumption;
- Athletes who drink to excess appear to do so at the well-intended advice of others to keep hydrated; and
- Recovery is rapid when hypertonic (3–5%) saline is given, but 0.9% saline is ineffective.
Despite growing evidence of the dangers of overhydration, in 1991, the United States Army developed guidelines (Burr, 1991) that mandated recruits drink 1.8 liters/almost 61 fluid ounces of liquid per hour when the temperature was 30 degrees Celsius/86 Fahrenheit or greater. This unfortunate mandate resulted in 125 hospital admissions for EAH and at least six fatalities attributed to it (Gardner, 2002; Garigan, 1999; O’Brien, 2001).
Apparently unaware of the above evidence and the now-six-known fatalities related to overdrinking during exercise, the American College of Sports Medicine published a new position statement in 1996 (Armstrong, 1996; Convertino 1996) that encouraged athletes to drink “as much as tolerable” during exercise. It was these guidelines that were in place at the time of the deaths of Cynthia Lucero and Hillary Bellamy. In 2007, they were revised (Sawka, 2007) to specify that athletes should replace the fluid they lost and not beyond.
From 1998 to 2007, there were four total deaths in marathon runners. And the development of low sodium during long-distance running was found to be anything but uncommon. In one study (Cairns, 2015), 70% of ultramarathoners were found to develop EAH during the course of the 100-mile race, The Great North Walk Ultras. And it is certainly not limited to ultramarathons. Yoga, for example, is one lower-intensity activity where practitioners are encouraged to drink excessive amounts and complications have occurred as a result (Reynolds, 2012; Bailowitz, 2016).
Physiology
Why does hyponatremia occur, and what is it about exercise that makes it much more likely to occur?
First of all, under normal physiologic circumstances, hyponatremia (low salt, or, better stated, excess fluid) does not occur. The salt-fluid balance in the human body is very tightly regulated. When your salt level begins to rise, you get thirsty, and normally humans have access to fluids, but if you don’t, your body will hold onto the fluid that is already in your body and your urine will become very concentrated. The opposite occurs on the rare occasion that a human is overhydrated: you will urinate a lot of dilute urine to get rid of the extra fluid. This is so rare, though, because it is uncomfortable to drink when you are already excessively hydrated.
This system can go haywire when the body is under extreme stress (respiratory failure, certain cancers, certain drugs, as well as during exercise and rhabdomyolysis) and this is called Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH). Again, SIADH is when the antidiuretic hormone (ADH) is not released in response to dehydration, but in response to stressors in the body.
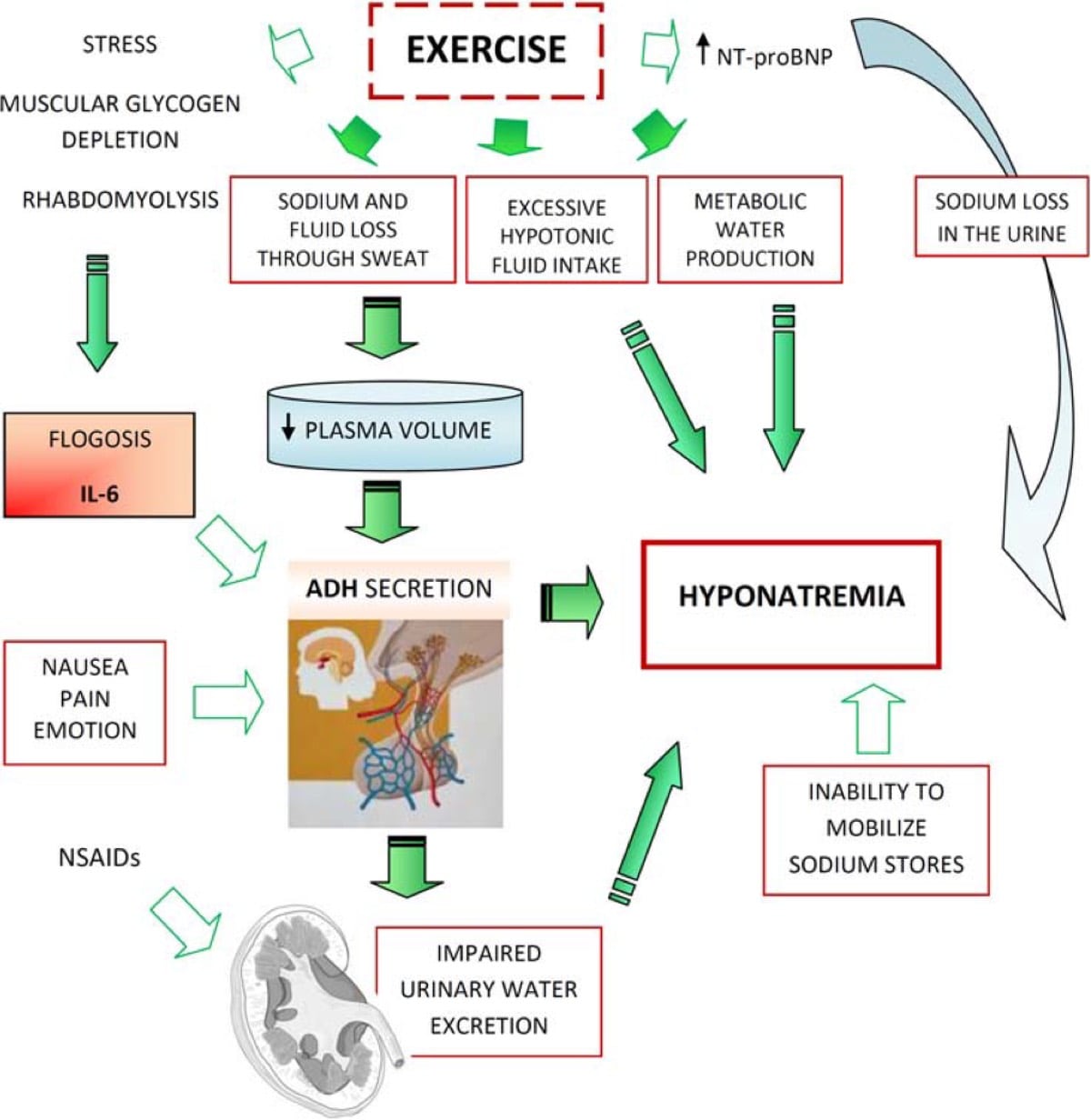
Figure 4. The current mechanism believed to be behind the development of exercise-associated hyponatremia (Urso, 2014).
Flogosis, or phlogosis: Inflammation.
NT-pro BNP: The N-terminal pro b-type natriuretic peptide is released in the blood when there is stress to the heart.
Hypotonic fluid: Fluid that has lower tonicity/concentration than normal human blood and thus causes swelling of cells and tissues—think reverse pickling.
It should be noted that the relationship between rhabdomyolysis and hyponatremia appears to be that of a vicious cycle where ‘rhabdo’ can lower sodium and low sodium can induce rhabdo. (Ellis, 2009; Bruso, 2010; Hoffman, 2015)
In exercise, again likely due to SIADH, humans tend to inappropriately secrete AVP/ADH, which holds onto the fluid you have, so you concentrate your urine even when you are not dehydrated. In other words, the fluid you drink stays in your body. Perhaps this is truly not something ‘going wrong’ during exercise, but is a strong protective mechanism to help you avoid dehydration.
The SIADH that occurs during exercise is not a problem unless humans start drinking a lot, specifically when they are not thirsty. In this unfortunate circumstance, the body just continues to secrete AVP and, instead of peeing out the extra fluid, the fluid builds up in the blood and tissues, and the sodium level in our blood drops. This drop in sodium in the blood is particularly problematic for the brain because water will be transported (through osmosis; again, think the reverse of pickling) to the brain, causing swelling. This is why weakness, seizures, and brain death can occur.
Symptoms
Initially the runner will notice they are no longer thirsty, likely become nauseated and/or experience a headache or become confused. A headache is a very rare symptom for a runner to have and should immediately raise the suspicion of hyponatremia. Unfortunately, oftentimes aid-station volunteers or a runner’s crew mistake this for dehydration and encourage the athlete to drink more, despite the athlete sometimes being adamant about not wanting to drink more. If drinking continues (even if the athlete has taken salt tablets), loss of muscle control and weakness can be seen.

Figure 5. Evidenced-base treatment options for exercise-associated hyponatremia associated with mild (yellow), moderate (orange), or severe clinical signs and symptoms (Hew-Butler, 2017).
Obtundation: Decreased level of alertness.
Dyspnea: Difficulty breathing, in this case it would be due to fluid building up in the lungs.
Decorticate posturing: When an unconscious person curls up into the fetal position.
Mydriasis: Dilated pupils.
We have all seen the videos of athletes stumbling all over the place or crawling to reach a race’s finish line. While most of the world seems to view this as ‘heroic,’ I and likely others familiar with EAH see this as a person with severe hyponatremia who now has swelling of the brain bad enough to lead to incoordination and muscle weakness, and is on the verge of seizures, coma, or death. This is what I think of when I see the images of 29-year-old Hyvon Ngetich crawling to third place at the 2015 Houston Marathon.

Figure 6. Image is a screenshot from a KXAN video of Hyvon Ngetich crawling across the finish line to finish third at the 2015 Houston Marathon. (In full disclosure, I do not know what her post-race sodium level was, but the way she loses muscle control and coordination in her legs and needs to crawl is strikingly similar to that seen in a video of Brian Morrison, who was known to have exercise-associated hyponatremia (EAH) with critically low sodium measured at a nearby hospital after he crossed the finish line at the 2006 Western States 100. Though the symptoms, such as confusion, associated with exertional heat stroke can be similar to that of EAH, an important distinction is that runners with heat stroke should not lose coordination or control of their muscles, as is shown in these videos. That loss of coordination is due to swelling of the brain and would not be expected in heat stroke. If temperatures are hot and heat stroke is suspected, a rectal temperature in excess of 104 degrees Fahrenheit/40 Celsius would confirm heat stroke. Please see Liza Howard’s heat-illness article for more information. If EAH is suspected, this can be confirmed or ruled out with an i-STAT machine, explained later in this article).

Figure 7. Image is a screenshot from a Fleet Feet Seattle video of Brian Morrison on the Placer High School track about to win the 2006 Western States 100. He lost control of his legs to the degree that he was helped across the finish line, disqualifying him from the win. Brian survived this medical incident.
Prevention and Treatment
I have heard people say various iterations of if only ultrarunners ‘kept up’ on their salt tabs, pills, or other means of ingesting supplementary sodium, finishes like that of Brian Morrison would never happen. But I think there is good reason to question this. Sodium supplementation during a 100-mile race has not been found to be related to the prevention of hyponatremia (Hoffman, 2015), or the prevention of cramping for that matter, but low sodium levels in the blood are instead related to fluid retention (Hoffman, 2015). It should truly be viewed as a problem with fluid and not a problem with salt. I think Hew-Butler et al. said it very well in their 2017 EAH review that, “It is the amount of fluid ingested rather than the amount of sodium ingested during exercise that drives the final blood sodium concentrations.”
The sodium level in the blood is exceptionally tightly controlled through innate mechanisms in the human body, which includes the ability to mobilize sodium from internal stores (such as the gut and bone) when needed. Indeed, runners can finish the Western States 100 (WS 100) without sodium supplementation and not develop EAH (Hoffman, 2015). Basically, when people take salt tabs, they tend to keep drinking and, rather than peeing out the fluid, their body bloats up. Sure, one could take salt tabs and drink nothing, but the tabs would be really hard to swallow and likely stimulate nausea (which in itself can lead to low sodium levels).
Based on available research (Hew-Butler, 2017; Hew-Butler, 2015; Hoffman, 2013; Hoffman, 2015) and my personal experience with salt tabs, if I were to run the WS 100, I would plan to drink and eat according to thirst and hunger and then go for salty foods if I felt like it. At this time, there is insufficient evidence to suggest that salt tablets are necessary to prevent EAH, even in an ultramarathon, and, in fact, they may come with risks.
That being said, there have also been many runners who have had record-setting ultramarathon finishes who did take salt tabs. Andy Jones-Wilkins, a seven-time consecutive WS 100 top-10 finisher reports having good success with sodium supplements, taking “600-800 milligrams of sodium per liter of fluid and increasing to 1,000 milligrams per liter of fluid in very hot (over 110 degrees Fahrenheit) conditions.” He continues to use this strategy today.
Camille Herron, the 2017 winner of Comrades Marathon and current holder of the women’s 100-mile world record, reports using a different strategy: “I tried taking salt tablets during long runs for a while, and it made me feel weird and crash and burn… What works for me is to use the salt shaker on foods and sip sports drink and water leading up to races. Then, during the race I carry a water bottle and a sports-drink bottle. I sip on both as needed. My gels have salt in them too—I take a gel with water every 30 minutes, and then sip on the sports drink in between. One thing I’ve learned is I feel the best taking a drink or supplement with potassium/magnesium/calcium in it—I think it helps to keep me peeing and the muscles firing!”
With these two examples, one can easily see that runners can have success with or without salt tablets. However, my review of the literature leads me to believe that taking salt tabs for sodium is more likely to cause problems than using a mixture of electrolyte drink and (potentially salty) food.
One incredible published example of sodium-tab supplementation gone wrong is this is that of a man who had previously developed EAH and was advised by his physician to take upward of 6 grams of supplemental sodium during a 72k run. At the finish line, emergency services were called because of this gentleman’s condition, and despite having taken in excess of 6,500 milligrams of supplemental sodium, his blood sodium level was critically low at 122 mEq/L (Hoffman & Meyers, 2017). This case elegantly demonstrated that EAH absolutely can develop despite ingesting large quantities of sodium.
One should also consider the potential side effects of sodium supplementation which are not limited to bloating and swelling but may include high blood pressure. I am personally aware of one runner who started taking salt supplements prior to his race and, in the pre-race medical screening, was found to have a blood pressure so high that he was not allowed to start the race. Granted his blood-pressure elevation may have been related to other factors, but ‘preloading’ with salt tabs could easily have raised it above the acceptable limit. This is truly something to keep in mind if you have an underlying diagnosis of high blood pressure.
Fortunately, prevention of EAH is very simple: drink when you are thirsty. And I advise drinking (and eating) whatever you are craving: water, sports drink, food, salt or not. Go for it, and let your body be the guide. Though there has been some recent debate about whether or not ‘thirst’ is as reliable during exercise as it is at rest. After reviewing the literature presented in Keneflik’s 2018 review, the argument that drinking to thirst does not do well to prevent dehydration during exercise is based on the fact that subjects who drink to thirst tend to lose weight. As discussed below, weight loss is an expected consequence of endurance exercise and suggests to me that thirst does indeed work correctly during exercise to prevent both hyponatremia and hypernatremia. Further, blood sodium level should be used as an indicator of whether or not drinking to thirst works rather than weight change during exercise.

Figure 8: Recommended strategy for avoidance of hyponatremia and dehydration (Hew-Butler, 2015).
Osmolality: The concentration of a solution, or the number of soluble particles per unit kilogram. Sodium and potassium, paired with chloride, are examples of soluble particles in the blood.
As discussed above, the treatment of EAH with brain dysfunction is with IV hypertonic (3%) saline. The treatment algorithm is shown in Figure 5.
Of note, physicians have historically been hesitant to give hypertonic 3% saline because it has been found to cause brain damage. (This occurs via central pontine myelinolysis, which is when the center of the part of the brain stem called the pons is severely damaged due to rapid movement of particles across the neurons’ protective cells, which is due to rapid correction of sodium levels in a person who has chronically low blood sodium. In these people, their brain has adjusted to being in something of a chronically swollen state.) For this reason, most doctors are taught to not use hypertonic 3% saline in anyone with low sodium. However, it takes the brain over 48 hours to reach the same sodium concentration as the blood. So for runners with EAH, the brain still has a close-to-normal sodium concentration, and you can correct the blood sodium as quickly as possible. So, please, especially those of you in health care, spread the word about hypertonic 3% saline (Hew-Butler, 2017; Noakes & Speedy, 2006). As you can see in Figure 5, it is the recommended treatment of EAH for athletes with the most severe symptoms (Hew-Butler, 2017).
Finally, physicians have been hesitant to give hypertonic 3% saline when a runner has elevated creatine-phosphokinase (CPK) consistent with rhabdomyolysis, but a CPK rise is expected after a long-distance running event (learn more in our rhabdo article) and should not delay or prevent administration of hypertonic 3% saline in cases of EAH. To reiterate, 0.9% saline treatment has been found to prolong recovery and may fail, and has likely failed, to save lives.
What We Have Learned at the Western States 100
I started working on research and in the finish-line medical tent of the WS 100 in 2013 and, that year, we were prepared to see EAH thanks to the research efforts of Marty Hoffman and Tamara Hew-Butler, both of whom are well known California-based physician researchers in ultra-endurance sports with extensive research experience at the WS 100. Marty even had a teaching session with me, where he showed me the video of Brian Morrison.
It was a hot year in 2013 and, even in the early morning, it was too warm to stand out in the rising sun. We received report of a runner at who was down at Brown’s Bar (at about mile 90), shaking and possibly having a seizure. He was transported by ambulance to the finish-line medical tent where he now clearly had developed seizures and (without knowing his blood sodium level) 100 milliliters of IV hypertonic 3% saline was administered. The runner stopped seizing and his mental status returned to normal. When he was admitted to the hospital, his sodium was still critically low at 122. We calculated that he likely had been as low as 119 before the hypertonic 3% saline. This was such a vivid example to me of how such a simple intervention can save a life. He did survive and ran again the next year (Thornley, 2014). However, unfortunately, his 2013 hospital stay was prolonged, apparently due to the refusal of the treating hospital to continue to use hypertonic 3% saline to normalize his sodium. (They used 0.9% instead.) This was due to concern for rhabdomyolysis, which was likely unfounded, again due to what we know about CPK levels in ultrarunners. As a side note, this runner reported that he had taken one salt tablet every 30-45 minutes during the race, but rather than preventing hyponatremia, it promoted weight gain. (He was up four pounds from his pre-race weight at the Rucky Chucky aid station, at mile 78.)
Historically, runners were weighed at the WS 100 aid stations and forced to drink if they were losing weight. Reportedly, runners put rocks in their pockets to avoid being pulled or stopped and told to drink more. This was purportedly begun to avoid dehydration in runners. By 2013, we did not use weight as a diagnostic tool at the WS 100. This was because of knowledge of the dangers of EAH and fluid retention as well as the research that had shown that weight does not always correspond to sodium levels (Hoffman, 2013). However, a couple good rules of thumb are:
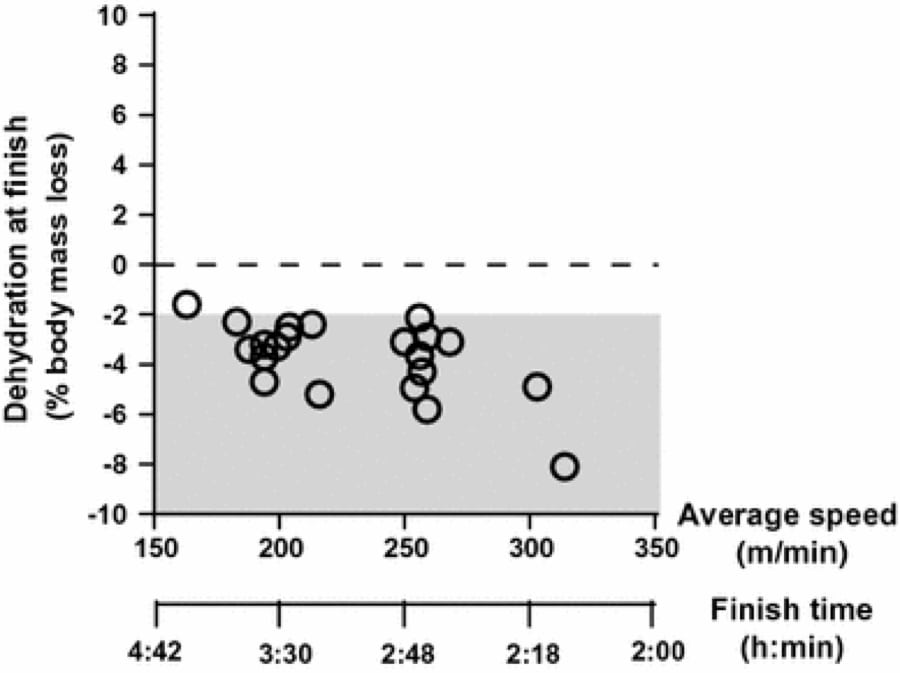
- Runners are expected to lose weight over the course of a 100-mile race, and a runner who has not lost weight is likely overhydrating; and
- There is actually a significant correlation between faster finishing time and more weight loss. The fastest runners can lose up to 5-7% body weight over the course of 100 miles without developing medical issues (Hoffman & Hew-Butler, 2013; Hoffman, 2013). That being said, as shown in Figure 10, a number of slower runners lost weight in excess of this, which was likely not beneficial. Additionally, we do not know the weights of runners who did not finish, though it stands to reason that excessive weight loss or gain would likely be associated with an increased risk of not finishing. However, mild weight loss was seen in the best performers.
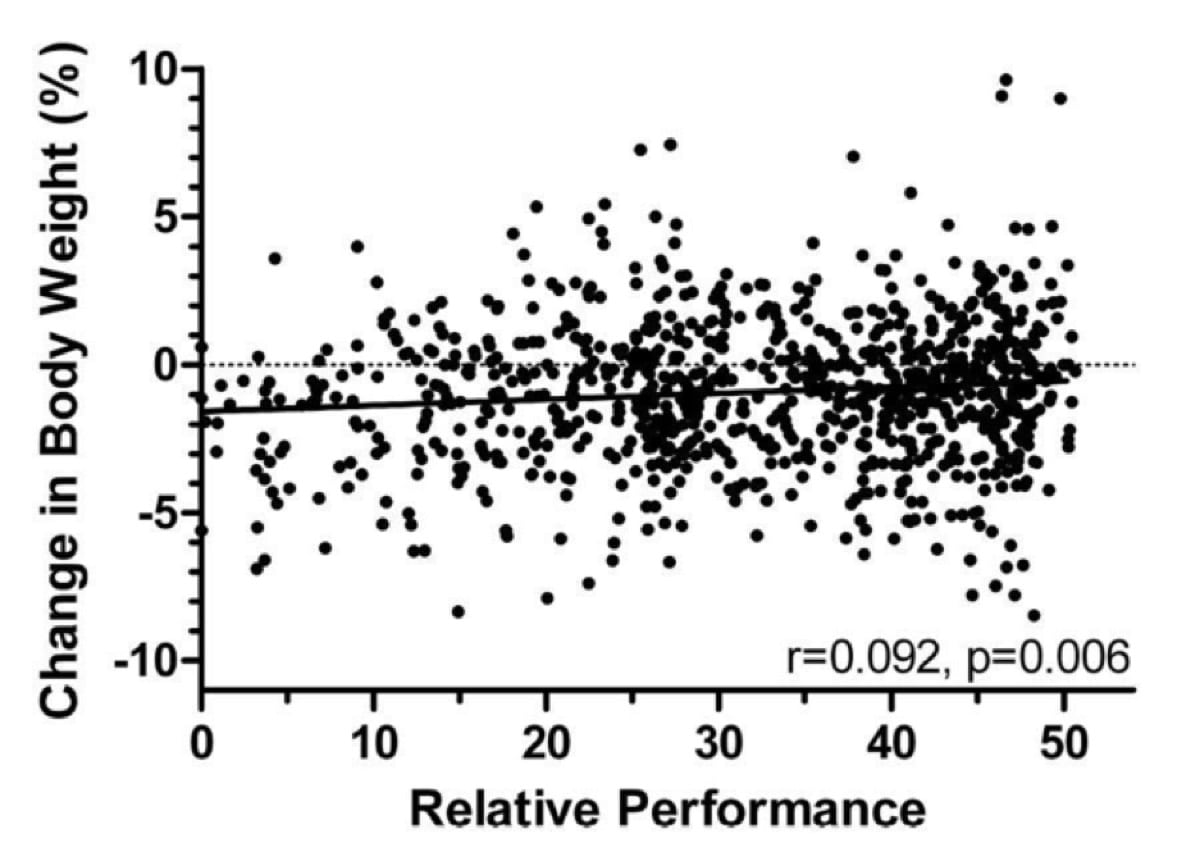
Figure 10. Change in body weight relative to performance at the 2009 Western States 100 (Hoffman, 2013).
A similar trend was also reported in marathon running, with the fastest finishers losing the highest percent body mass (Cheuvrant, 2007).
By 2014, we ditched the scales entirely at the WS 100 (in 2013 they were only used for research purposes) and instead told the runners to drink if they were thirsty, but not according to a schedule or at the encouragement of others.

Figure 12. A 2013 Western States 100 runner feeling light and free at Robinson Flat, mile 30, knowing he would not be pulled from the race or told to hydrate because of his weight. Photo: Tracy Beth Høeg

Figure 13. The 2017 Western States 100 research team including Brian Toedebusch, Ali Warrick, Tracy Høeg, and Sarabeth Maciey in the finish-line medical tent getting ready to draw blood from participating finishers. Photo: Tracy Beth Høeg
At the 2017 WS 100 (Figure 13), post-race blood sodium levels were checked as part of the metabolomics of performance study (Høeg, 2018). What we found was surprising and encouraging: only 1/30 (3.3%) of runners participating in our study had hyponatremia post-race, and the one who did had a borderline low sodium of 134 mEq/L. This was in stark contrast to the 30% (14/47) found at the 2009 race (Hoffman, 2013). Though it is difficult to draw conclusions based on these results, it suggests that WS 100 runners are currently using more effective hydration strategies than in the past.
The i-STAT
A helpful tool called the i-STAT allows for immediate laboratory analysis on site at a race. This is something we have used the last couple of years at the WS 100 and it has eliminated doubt about whether or not a participant has EAH. This is something all major races could consider purchasing especially if there is a concern for frequent EAH.
Conclusions
- Overdrinking (water, sports drink, or other hypotonic fluid) can be deadly during exercise.
- Hyponatremia presents initially as headache, nausea, vomiting, and an aversion to fluids, and it progresses to muscle weakness and incoordination, seizures, and brain death due to brain swelling.
- Severe hyponatremia should be treated with cessation of exercise and hypertonic 3% saline IV fluids. Mild hyponatremia can be treated with oral hypertonic fluids.
- Runners should drink to thirst and not beyond, and their supporters should support and recognize this.
Now, go enjoy a cold beverage on me! It’s hot out there.
Call for Comments
- Do you have a personal experience with exercise-associated hyponatremia that you would like to share?
- If yes, what lessons did you learn and how did you adjust your hydration strategy?
References
Bruso JR, Hoffman MD, Rogers IR, Lee L, Towle G, Hew-Butler T. Rhabdomyolysis and hyponatremia: a cluster of five cases at the 161-km 2009 Western States Endurance Run. Wilderness Environ Med (2010) 21(4):303–8.
Burr R E. Heat illness: a handbook for medical officers. Natick, MA: US Army Research Institute of Environmental Medicine, 1991
Cairn RS, Hew-Butler T. Incidence of Exercise-Associated Hyponatremia and Its Association With Nonosmotic Stimuli of Arginine Vasopressin in the GNW100s Ultra-endurance Marathon.Clin J Sport Med. 2015 Jul; 25(4):347-54.
Cheuvront SN, Montain SJ, Sawka MN. Fluid replacement and performance during the marathon. Sports Med. 2007;37:353–7.
Ellis C, Cuthill J, Hew-Butler T, George SM, Rosner MH. Exercise-associated hyponatremia with rhabdomyolysis during endurance exercise. Phys Sportsmed (2009) 37(1):126–32.
Gardner J W. Death by water intoxication. Mil Med 2002167432–434.
Garigan T P, Ristedt D E. Death from hyponatremia as a result of acute water intoxication in an Army basic trainee. Mil Med 1999164234–238.
Hew-Butler T, Roser MH, et al. Statement of the Third International Exercise- Associated Hyponatremia Concensus Development Conference, Carlsbad, California, 2015. Clin J Sport Med. 25 (4) 7.
Hew-Butler T, Loi V, Pani A, Rosner MH. Exercise-Associated Hyponatremia: 2017 Update. Frontiers in Medicine. 2017;4:21. doi:10.3389/fmed.2017.00021.
Hoffman M & Hew-Butler T. Weight change During a 100-Mile Race. Ultrarunning Magazine. https://ultrarunning.com/features/weight-change-during-a-100-mile-race/ 11/24/2013. Accessed 8/3/2018.
Hoffman M. D., Stuempfle K. J., Rogers I. R., Weschler L. B., Hew-Butler T. (2012b). Hyponatremia in the 2009 161-km Western States endurance run. Int. J. Sports Physiol. Perform. 7, 6–10.
Hoffman MD, Stuempfle KJ, Sullivan K, Weiss RH. Exercise-associated hyponatremia with exertional rhabdomyolysis: importance of proper treatment. Clin Nephrol (2015) 83(4):235–42.
Hoffman MD, Hew Butler T, Stuempfle K. Exercise-Associated Hyponatremia and Hydration Status in 161-km Ultramarathons. Medicine & Science in Sports & Exercise 2013; 45(4): 784–791.
Hoffman MD, Myers TM. Case study: symptomatic exercise-associated hyponatremia in an endurance runner despite sodium supplementation. Int J Sport Nutr Exerc Metab (2015) 25(6):603–6.10.1123/ijsnem.2014-0241
Hoffman MD, Stuempfle KJ. Sodium supplementation and exercise-associated hyponatremia during prolonged exercise. Med Sci Sports Exerc (2015) 47(9):1781–7.
Kenefick, R.W. Sports Med (2018) 48(Suppl 1): 31.
Noakes TD, Goodwin N, Rayner BL, Branken T, Taylor RK. Water intoxication: a possible complication during endurance exercise.Med Sci Sports Exerc. 1985 Jun; 17(3):370-5.
Noakes TD, Speedy DB. Case proven: exercise associated hyponatraemia is due to overdrinking. So why did it take 20 years before the original evidence was accepted? Br J Sports Med. 2006 Jul; 40(7): 567–572.
O’Brien K K, Montain S J, Corr W P. et al Hyponatremia associated with overhydration in U.S. Army trainees. Mil Med 2001166405–410.
Orton, K. 2006. Woman Dies Two days after running in Marine Corps Marathons. https://www.washingtonpost.com/archive/sports/2002/10/31/woman-dies-2-days-after-running-in-marine-corps-marathon/5766eb4e-30d4-4321-97e6-efd6cf071e13/?utm_term=.7f2a779e9058
Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc. 2007 Feb;39(2):377-90.
Siegel AJ et al. Hyponatremia in Marathon Runners due to Inappropriate Arginine Vasopressin Secretion. Am J of Sports Med. (2007) 120, 461.e11-461.17.
Smith, S. Marathon runner’s death linked to excessive fluid intake. 8/13/2002. The Boston Globe. https://www.freerepublic.com/focus/news/732350/posts
Thornley C. “Medical Needs at Ultra-Endurance Footraces: Race Director’s Perspective.” 6/25/2014. 2014 Medicine & Science in Ultra-Endurance Sports Conference. Squaw Valley, USA.