Maybe your social media feed looks a little like mine, flooded with athletes preaching the benefits of some new, super recovery aid. They’re being compressed, poked, prodded, frozen, vibrated, stretched, rubbed, rolfed, stimulated, elevated, mashed, and lightly bludgeoned. They’re using gadgets that may cost hundreds to thousands of dollars or even going to special recovery studios. We are told, “if we are training hard, then we should be recovering even harder.” What was once a passive act of simply not training has become something we actively do. Simply said, exercise-recovery modalities are a huge trend.
In this article, we discuss what recovery means in the context of run training. We also break down some popular recovery modalities to see how effective they are–and aren’t–according to the current scientific literature. In this article, we explore massage, compression, foam rolling, electrical stimulation, cold-water immersion, whole-body cryotherapy, active recovery, proper nutrition and hydration, and rest. We can’t cover all of the modalities, so we close this article with recommendations on how each of us can best navigate the wild world of exercise recovery.
The Goldilocks Principle of Training and Recovery
Adequate stress plus adequate rest equals positive physiological adaptation. This is the basic principle of training. Those miles and hours you log as you prepare for your goal race, when combined with recovery runs, rest days, and recovery weeks, should lead to a steady progression over a season. Ideally, this culminates in a great day where you tackle your performance goal. See what I did there? I put training and recovery on equal footing.
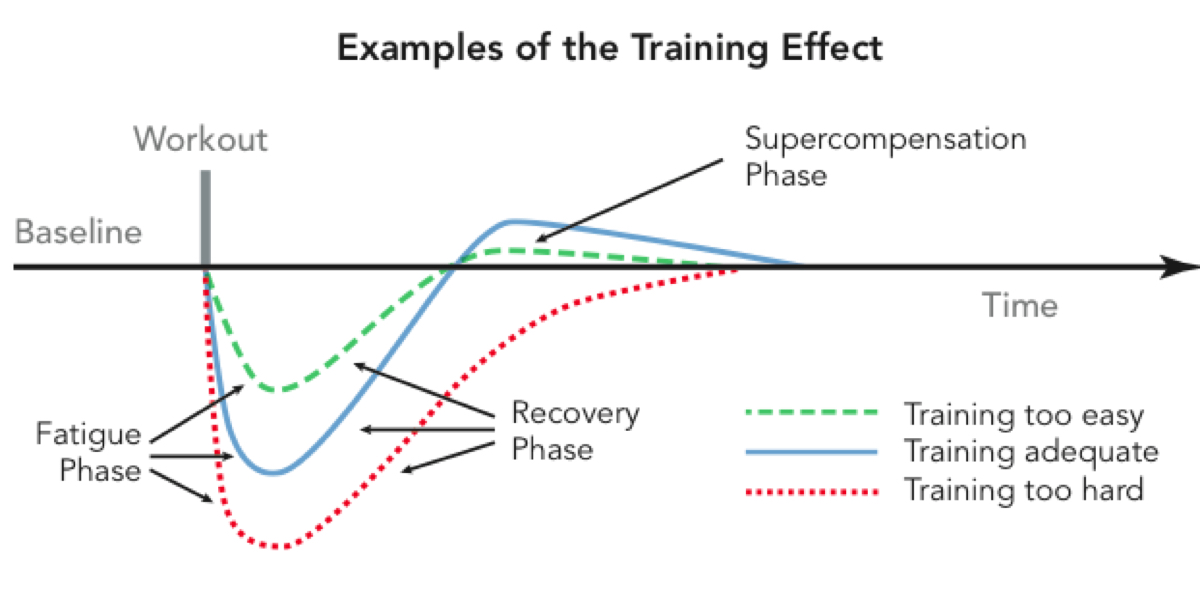
Figure 1. Training is a balancing act of just enough training followed by just enough recovery. This basic principle, when repeatedly applied to a training season, should maximize your fitness. Image: Rockandice.com/rock-climbing-training/the-training-effect-steve-house-and-scott-johnston/
The wise Joe Friel once wrote, “A hard workout only creates the potential for fitness. It’s realized when you recover afterwards” (1). Recovery is the time period where the physiological adaptations occur. During this time, our bodies repair the cellular-level muscular damage exercise causes, expand our capillary beds (where oxygen transfers from our blood to our tissues), increase our mitochondria (the place inside our cells where energy is produced), and restore homeostasis (multi-systemic balance) (2). When successfully carried out, this adaptation period readies our body for the next physically stressful workout or week. The real questions then become, how long is that necessary recovery period and can we speed it up? These questions drive the recovery-modality market as we try to make recovery ‘better.’
We know that exercise, particularly long-distance trail running with its eccentric movements, causes muscle damage. This damage likely causes tissue inflammation, an increased sense of perceived fatigue, and–everyone’s personal favorite–delayed-onset muscle soreness (DOMS). All of these results limit performance (2). Recovery tools, tricks, and treatments target this space, and predominately attempt to limit inflammation by increasing blood flow in our bodies through various means.
We importantly note that recovery tools’ psychological effects have not yet been deeply explored by the scientific literature. A lot of tools likely make athletes feel better simply because they believe they are doing something proactive. And many recovery tools make a person sit still and relax, which can in turn release beneficial hormones. Positive sensations are positive, however they are achieved, so there’s nothing wrong with a positive placebo effect.
Beyond the subjective measure of how you feel, we can now monitor our bodies’ recovery from exercise via biochemical markers. These biomarkers are creatine kinase (a protein released into the bloodstream when muscles are damaged) as well as c-reactive protein and interleukin-6 (proteins released into the blood when tissues are inflamed) (2, 3). By measuring their levels in the blood before and after using a recovery tool, we can in theory evaluate the tool’s effectiveness.
Finally–and this is really important–it’s hard to create a blinding placebo in the testing of many recovery modalities. For example, you can’t replicate cold water that isn’t cold or cause electrical stimulations that do not actually stimulate. This causes problems when testing the effectiveness of recovery tools in research because you can’t rule out a placebo effect. Thus, we must understand that confounding variables may be present in this research.
Massage
What It’s Supposed to Do:
Massage is one of the most traditional recovery modalities athletes use. Massage theoretically reduces delayed-onset muscle soreness by increasing blood and lymphatic flow and reducing inflammation (2). More specifically, it’s thought that by increasing the circulation of blood and lymph you may be able to decrease the amount of creatine kinase in the blood (2).
What the Science Says:
The science of massage is mixed. To start, although massage in theory should increase blood and lymphatic flow, which should help clear metabolic waste, the scientific literature doesn’t support this. Not to lose hope entirely, a 2016 study suggested the best types of massage to increase blood and lymphatic flow are specifically effleurage and petrissage techniques. These techniques focus on light, long strokes working into deeper strokes to avoid the muscles tensing under increased pressure which increases relaxation and blood flow to the skin’s surface (10).
Massage is more promising when it comes to the subjective measure of immediate pain management. A 2018 meta-analysis (a research paper that does an exhaustive review of the scientific research on a subject to form a consensus statement) and a 2019 study looking at massage post-habitual exercise both show that massage can have a positive effect on how we feel pain (2, 4). In the 2018 meta-analysis, massage saw the strongest indication of moderating post-workout pain compared to other recovery interventions. And the 2019 study found the largest effect of massage on perceived pain occurred immediately post-massage. This may be due to massage’s scientifically understood neurologic component, that its mechanical stimulus inhibits pain by ‘closing’ neuropathways. (4).
The other reason–one that’s less highlighted in sports-performance research–massage is believed to aid in recovery is by decreasing our sensation of pain by increasing the release of beta endorphins (substances produced in the pituitary gland that reduce feelings of pain) and decreasing the release of stress hormones (5, 6). Specifically, massage has been linked to an increase in oxytocin (a relaxation hormone) and a decrease in the release of adrenocorticotropic hormone (a stress-response hormone) (26).
Finally, despite massage’s short-term effects being strongly supported by the scientific literature, the data on the effect of more delayed pain (72 hours after a workout) is not as strong.
What This Means:
Massage might temporarily make you feel better, but it might also primarily be an expensive, short-term, feel-good boost.
Compression
What It’s Supposed to Do:
Moon boots, compression boots, or puffy pants, you’ve likely seen a photo of an athlete lounging in a pair after a hard training day. Pneumatic compression, most commonly intermittent pneumatic compression (IPC) devices, apply intermittent and sequential compression to different compartments of an inflatable sleeve worn over the leg (or arm). The idea behind IPC is that the sequential pressure and compression alter localized blood pressures (often referred to as hemodynamics) and increase blood flow to expedite the removal of metabolic waste (9). IPC devices were originally developed for medical use in post-operative care to accelerate skin blood flow to help with healing.
We also have the more traditional compression garments such as running socks, tights, and calf sleeves. Compression garments were also developed for medical use to treat conditions like lymphedema (when the lymph nodes don’t properly drain), deep-vein thrombosis (a blood clot in the lower leg generally), and chronic venous insufficiency (difficulty moving blood back to the heart) (27).
In the athletic-recovery context, the scientific understanding is that wearing compression garments post-exhaustive exercise does two things:
- minimizes lower-leg swelling by helping lymph drainage; and
- aids in venous return (blood moving toward the heart) by decreasing major-vein diameter, which increases the velocity and volume of blood flow and limits venous reflux (blood moving away from the heart and pooling in the limbs) (28).
Note that inflammation and blood pooling in the limbs don’t occur via the same mechanism although they are both influenced by blood flow. Inflammation is an immune-mediated response where white blood cells are attracted to a site of tissue damage, and increasing blood flow aids in the movement of these cells. When it comes to blood pooling, venous return is the mechanism and compression helps fight gravity (28).
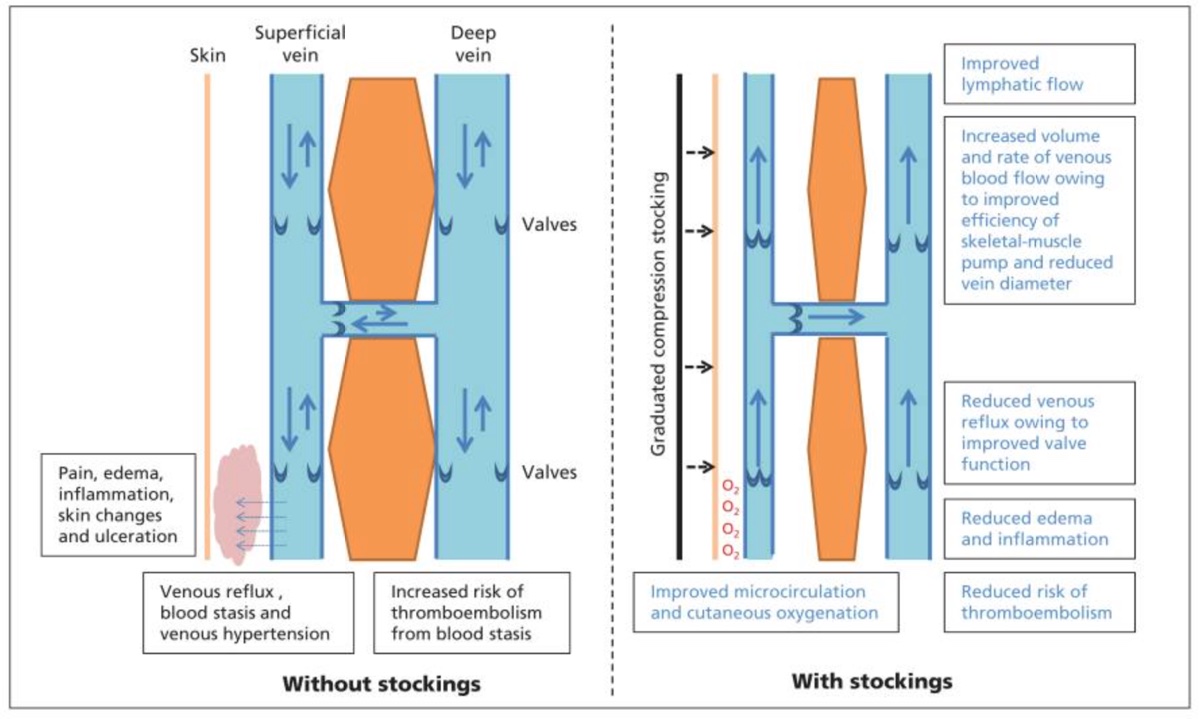
Figure 3. A scientifically validated rationale for how compression garments work is that they cause major veins to narrow, which then increases the velocity and volume of blood returning to the heart. This also allows the skeletal-muscle pump (a group of muscles that help blood circulate) to work more effectively. Compression garments also decrease venous reflux (blood moving away from the heart and pooling in the limbs) and blood stasis (stagnation). Image: Lim & Davies, 2014 (28)
What the Science Says:
In studies (8, 9, 2) conducted with healthy young men post-eccentric exercise including immediately post-ultramarathon, IPC devices only very slightly outperformed–this performance wasn’t statistically significant–massage or passive rest (laying horizontal for 20 minutes) for the reduction of creatine kinase, c-reactive protein, and interleukin-6. (9)
One of the ways compression garments have shown signs in the scientific literature of aiding recovery is by reducing the perception of fatigue and muscle pain, perhaps by reducing the physical space available for swelling and inflammation to take place and improving venous return (2, 11).
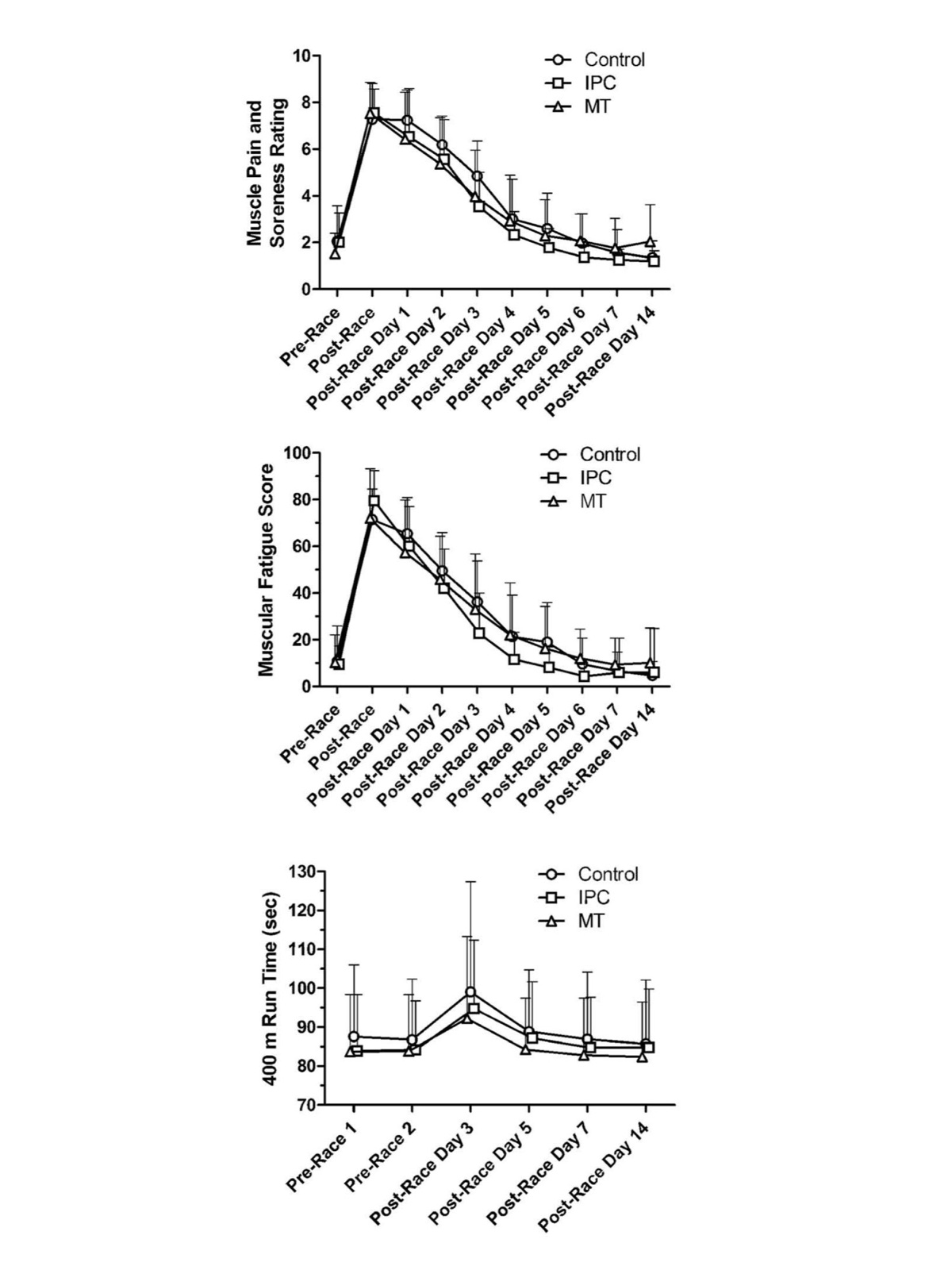
Figure 4. Participants completed a 62.7-kilometer, 87.4k, or 102.8k race during the 2016 Tarawera Ultramarathons, and then various recovery measures were recorded at units of time post-race. Participants were divided into three groups, those receiving massage therapy (MT), those using intermittent pneumatic compression (IPC), and a control group that remained horizontal for 20 minutes. There was no significant difference between the three groups over the course of the recovery period for the muscle pain and soreness rating, muscular-fatigue score, and a repeated 400-meter time trial (which was compared to a pre-race value). Image: Heapy et al 2018 (9)
What This Means:
The fancy, space-age boots and almost-impossible-to-get-on compression socks do not have a significant effect on recovery biomarkers. They have been shown to reduce perceived fatigue and muscle soreness for some people slightly more than passive recovery, though this difference isn’t statistically significant. So maybe it’s best to own a pair of compression socks and borrow a pair of inflatable pants.
Finally, current science tells us two more things:
- Compression garments are most effective post-exercise; and
- The amount of pressure exerted by compression garments on the legs is important, so make sure to buy the correct size (27).
Foam Rolling
What It’s Supposed to Do:
Foam rolling is an old favorite of many a runner. It hurts so it must be working, right? Foam rolling is essentially self-massage thought to improve performance by helping to increase flexibility and alleviate muscle fatigue and soreness (12). The potential positive effects of foam rolling are said to be many, including a reduction in tissue adhesion, a pain-mediating effect on the nervous system (like with massage), increased blood flow, and the psychological effects of improved perceptions of well-being due to the release of endorphins into your blood (again similar to massage) (12).

Figure 5. iRunFar Managing Editor Meghan Hicks foam rolling after exercise. Photo: iRunFar/Bryon Powell
What the Science Says:
While there are many bioplausible reasons (hypotheses that are unproven but in line with current scientific understanding) athletes have been told to foam roll, there is very little scientific literature to back any of them up. Wonderfully enough, a brand-new meta-analysis of 21 research articles studied the effects of pre- and post-exercise foam rolling on athletic performance and muscular soreness.
Foam rolling post-exercise produced mixed results in jumping, strength, and sprinting performances. There were some slight improvements, some slight impairments, and seemingly no clear-cut answer. One area where foam rolling post-exercise shines is in subjective muscular soreness. The meta-analysis suggests that 66% of the population is likely to experience muscle-pain reduction when foam rolling post-exercise (12).
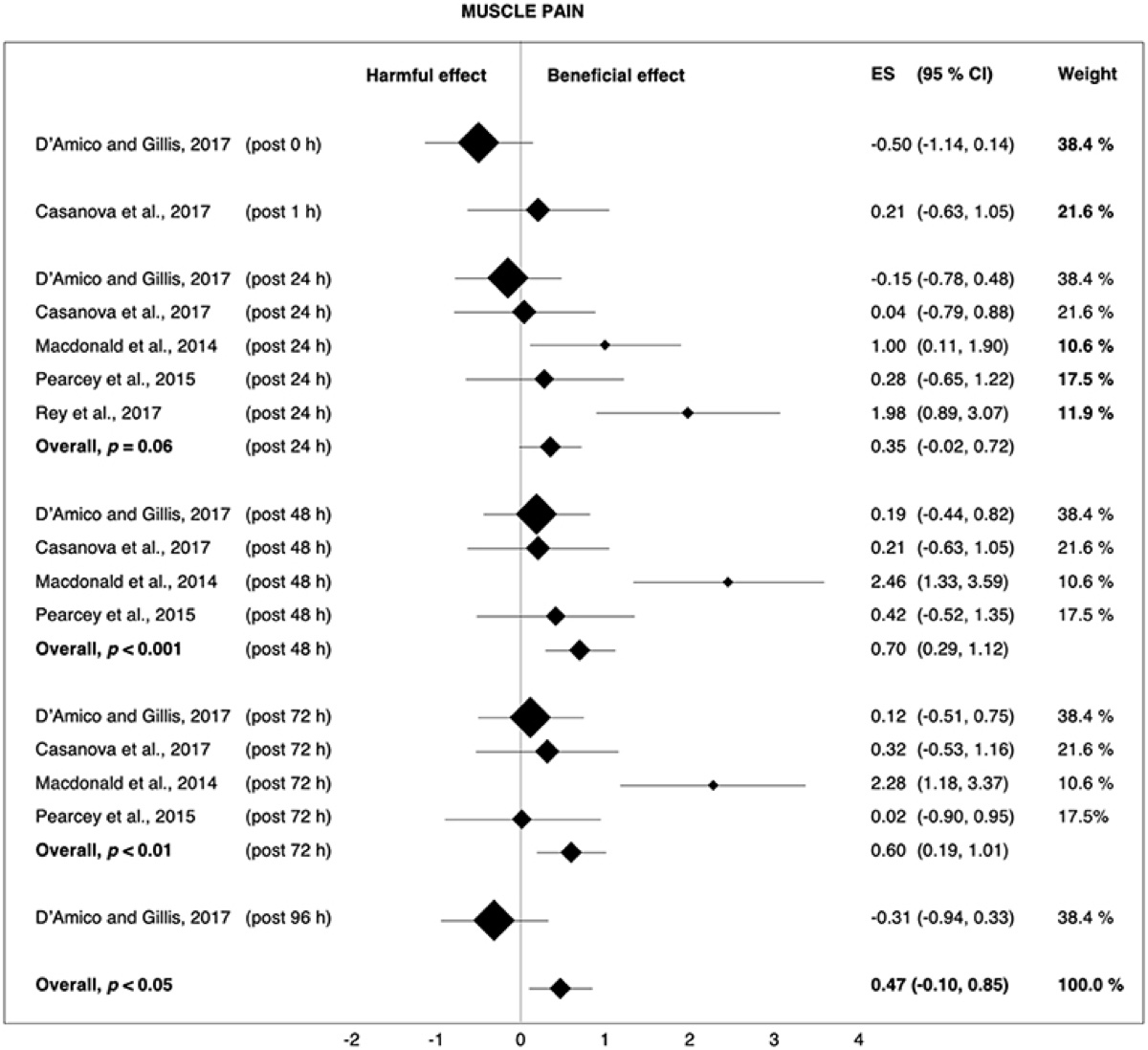
Figure 6. The graphic representation of a meta-analysis of the effects of post-exercise foam rolling on muscle pain. In the studies that looked at foam rolling post-exercise, a majority showed a reduction in muscular pain. The post value refers to how long post-foam rolling the muscular-pain survey was conducted. Some studies took multiple post-foam-rolling measures and found the most improvement 48 and 72 hours later. The weight of an individual study’s data on the meta-analysis is indicated by the size of the diamond in the graph; for example, a study with a large sample size would have a higher weight and is represented by a larger diamond. Image: Wiewelhove et al 2019 (12)
What This Means:
Foam rolling post-exercise is likely to reduce the perception of muscular soreness in a majority of athletes. Although this is a subjective measure, muscular pain can have real, negative consequences on performance. The decrease in muscular soreness from foam rolling is likely similar to massage in that you temporarily inhibit your pain sensation via mechanical pressure (12).
Electrical Stimulation
What It’s Supposed to Do:
Neuromuscular electrical stimulation (NMES) devices also come to athletics from the medical setting where they are used as an effective, non-pharmacological way of treating vascular disorders by increasing blood flow (14). So, in the athletic setting, the idea is that involuntary muscle contractions from a NMES device can increase blood flow and speed recovery by aiding in the flushing of metabolic waste (theoretically similar to massage and IPC).
You might have heard about another kind of electrical-stimulation device, transcutaneous electrical nerve stimulation (TENS). TENS targets sensory nerves, which send pain signals to the brain, while NMES targets the muscles themselves via motor nerves. In medicine, TENS is used to treat chronic pain by stimulating endorphin release (13). TENS isn’t used for exercise recovery and isn’t examined here.
Figure 7. Targeted advertising? A screenshot of the author’s Instagram feed showing an ad for a neuromuscular electrical stimulation device.
What the Science Says:
Despite it being easy to get behind idea of these muscular contractions stimulating blood flow and therefore improving recovery, scientific research on NMES devices has produced conflicted results (13, 14). Though using a NMES device is better than passive recovery at removing metabolic waste, it’s still not as effective as active recovery (cooling down immediately after exercise). This might be due to active recovery utilizing metabolites from the hard effort as fuel and continuing to actively circulate blood in a more whole-body way (17).
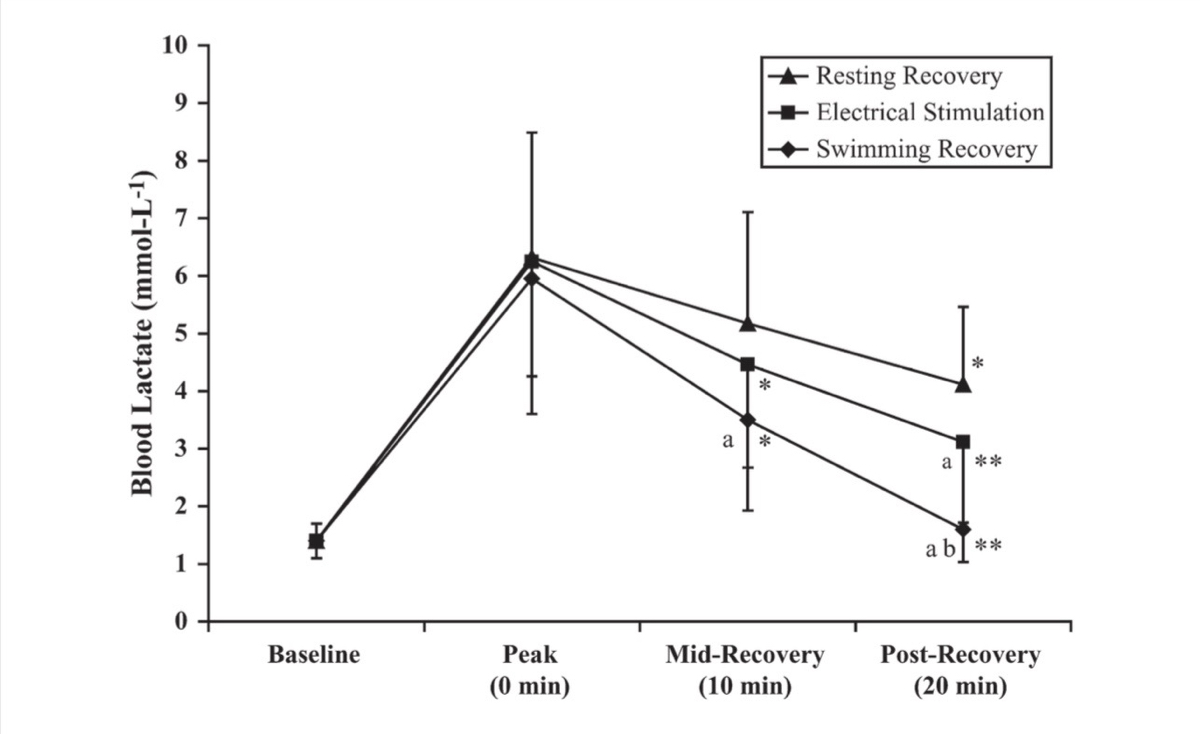
Figure 8. After swimmers completed 200-yard maximal efforts, they utilized three different recovery modalities: resting recovery (passive sitting), electrical stimulation (a neuromuscular electrical stimulation device on the upper body), and swimming recovery (100-yard repeats at 65% of maximum velocity for 20 minutes). Although electrical stimulation is better than passive recovery at clearing blood lactate (metabolic waste) at the 10- and 20-minute marks, it is not as good as swimming recovery. Image: Neric et al., 2009 (17)
What This Means:
Scientific research shows that active recovery is more effective than using a NMES device. This begs the question, why would anyone buy one? There are a few situations where the benefits might be worth it. For example, if you are unable to cool down effectively, maybe due to time restraints or you are trying to limit musculoskeletal-system impact, NMES becomes a good option. Another way to use it might be as a secondary recovery workout in lieu of a recovery run, spin, or walk because it has a lower metabolic cost.
Cold-Water Immersion
What It’s Supposed to Do:
Cold-water immersion (CWI)–or what every runner loves to hate, the ice bath–has three major, hypothetical mechanisms for boosting recovery. First, cold-induced vasoconstriction (the narrowing of blood vessels) might reduce the permeability of lymph vessels and capillaries (the ability for substances to cross cell membranes) which could reduce fluid movement. This decrease in fluid movement into our tissues would then limit inflammation (19). The second possibility is that a decrease in muscle-tissue temperature may slow injured tissue’s metabolic needs and avoid further injury, which should improve the healing process (19). Finally, it’s possible that a tissue-temperature decrease blunts nerve conduction, which then decreases our pain perception and reduces the possibility of muscle spasm in injured tissue (18, 19).

Kelly Wolf (left) and YiOu Wang recovering with an ice bath in the European Alps. Photo courtesy of YiOu Wang.
What the Science Says:
While we know that CWI has some selectively positive effects on recovery, we do not thoroughly understand the mechanisms behind them yet. A review article looking at CWI versus controls showed that CWI was not an effective means of recovering muscular strength post-exercise (19). However, it did indicate that 69% of the population would likely experience lesser sensations of delayed-onset muscle soreness after using CWI (19).
We are also learning that when and how we use CWI potentially impacts its effectiveness for recovery. There’s strong evidence that CWI has positive effects when used acutely, like to help you perform on back-to-back days or in a multi-round competition (18).
The scientific community has had a great debate over the past five years about the possible negative effects of CWI on long-term training adaptations. This fear has been focused on the understanding that the cellular and biochemical actions (namely inflammation) that CWI supposedly blunts are critical to physiological adaptation (18). The strength and conditioning world, which has put a lot of research into this topic, now shies away from ice baths altogether. The truth is, they’re not 100% wrong, but they’re not 100% right either.
Contrast-water therapy is another kind of water therapy where you move from an ice bath to a warm bath (about 94 degrees Fahrenheit/34 degrees Celsius) and back for 10 to 15 minutes. Contrast baths are thought to work similarly to CWI where the cold induces vasoconstriction, but then the warm water induces vasodilation. This repeated narrowing and widening of the blood vessels should theoretically improve blood circulation. At this time there is no scientific support for this mechanism’s objective performance, though it’s been shown that warm water subjectively has a ‘nice’ feeling on the joints (30).
What This Means:
Our present understanding of CWI is that it’s best used on days where you need to recover quickly to perform again in the short term. Using CWI in these moments could help maintain your training quality by lessening your feelings of muscle soreness. The rest of the time it’s likely best to let your body naturally process some of that inflammation and damage.
Additionally, the scientific literature suggests immersing in 51- to 59-degree Fahrenheit (11 to 15 Celsius) water for 10 to 15 minutes (29, 30).
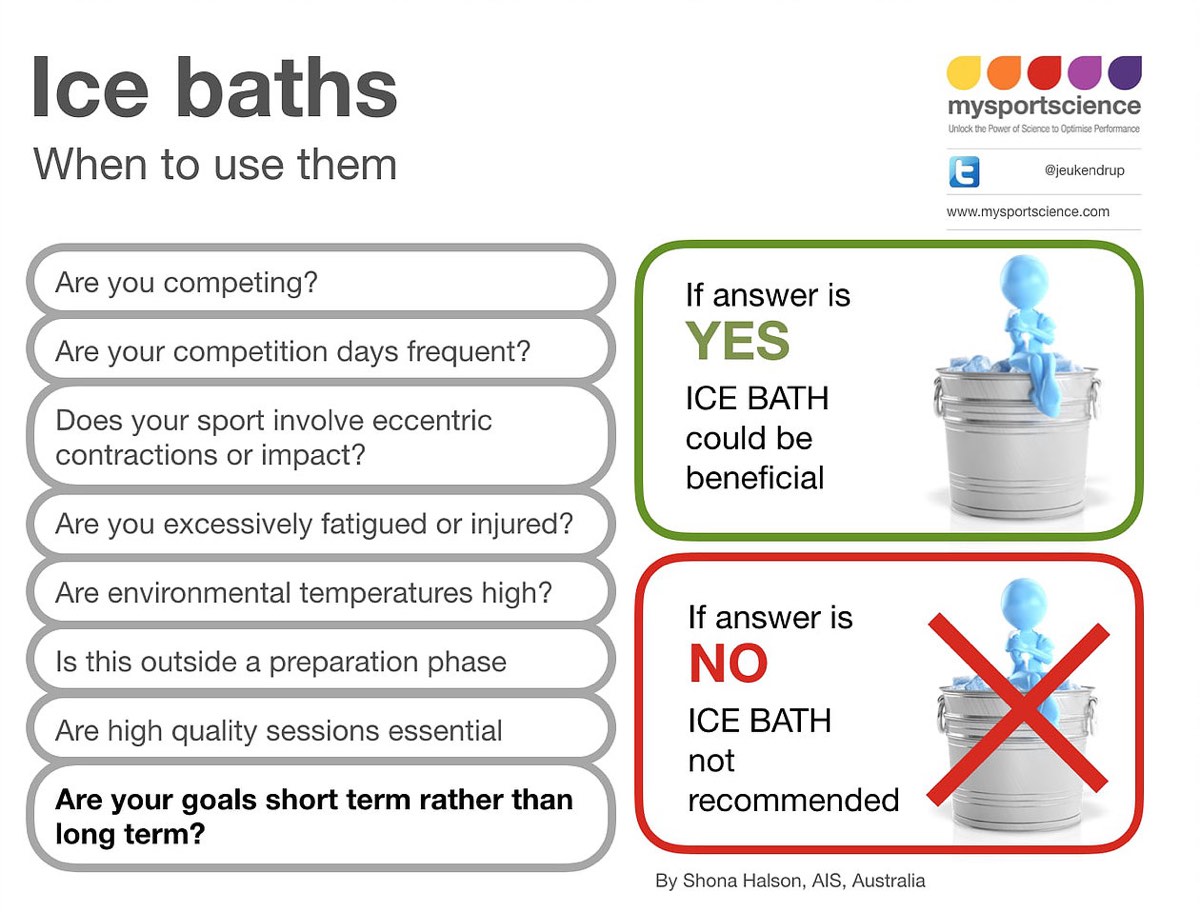
Figure 9. Context is key in deciding when to ice bath. The scientific literature currently recommends using this recovery modality only at specific times in order to boost short-term recovery while not inhibiting positive adaptations from training in the longer term. Image: Mysportscience.com/single-post/2016/06/16/Ice-Baths-for-Recovery-Black-white-or-somewhere-in-between
Whole-Body Cryotherapy
What It’s Supposed to Do:
Cryotherapy is a medical term for cold therapy (generally cooling localized areas of the body to blunt inflammation). Whole-body cryotherapy (WBC) is the ritual of standing for approximately three minutes in a chamber cooled to -166 to -220 Fahrenheit (-110 to -140 Celsius). To me WBC sounds like quite literally freezing to death, but for years people have proclaimed a host of positive effects. Akin to cold-water immersion, WBC’s premise is based on the idea that it blunts inflammation via cold-induced vasoconstriction. The question is, does it work?
What the Science Says:
Due to lots of mixed research results over the past decade, the jury is out on WBC. In the most recent studies, however, it appears that dosing is the variable that controls WBC’s effectiveness for recovery, specifically how many sessions and days in a row a person uses it.
In a 2019 study looking at an acute, one-time session of WBC after a strenuous trail run, there was no improvement in the hormonal, inflammatory, or muscle-damage biomarkers compared to passive rest. This is supported by a 2013 study that found no changes in circulating creatine kinase after athletes were exposed to either three or six sessions of WBC compared to passive recovery (24, 21).
In another study where participants took part in a total of 10 sessions over five days with repeated rounds of eccentric exercise, there was a decrease in bloodstream creatine kinase of approximately 30% despite continuing to do muscle-damaging exercise (25).
Finally, a 2018 study compared the effects of WBC, cold-water immersion, and a placebo (a cornstarch pill participants were told was branched-chain amino acids) on recovery. In measuring recovery objectively via muscular inflammation, the placebo outperformed both WBC and cold-water immersion. However, WBC edged out the other two treatments in subjective feelings of muscular pain post-exercise (20).
What This Means:
We don’t know yet if whole-body cryotherapy is an effective recovery tool. The latest research shows the need to potentially do two sessions a day (before and after exercise) to decrease post-exercise recovery biomarkers and feelings of muscle pain. I’m not sure any of us has the time or resources for that, so take it all with a grain of salt.
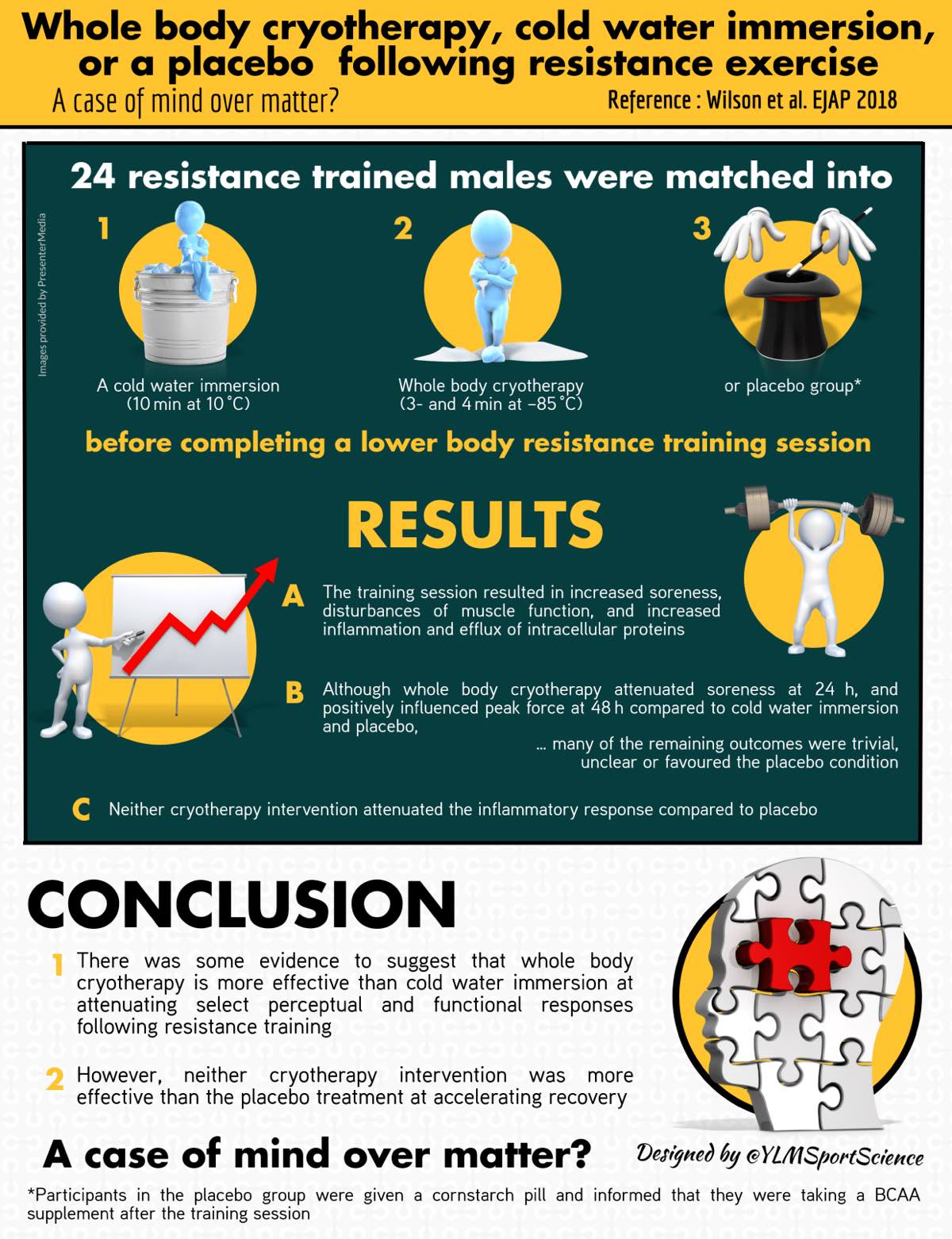
Figure 11. The mind is a powerful tool. This infographic shows the mixed results of a survey comparing the effectiveness of whole-body cryotherapy, cold-water immersion, and a placebo. Image: Ylmsportscience.com/2018/12/24/whole-body-cryotherapy-cold-water-immersion-or-a-placebo-following-resistance-exercise/
Active Recovery
What It’s Supposed to Do:
Active recovery, or a cool-down, is the act of continuing to move at a very easy effort for approximately 20 minutes following more intense exercise (31). The main rationale behind cooling down is that continued increased blood circulation helps to clear metabolic waste. This is because your body processes metabolites through oxidative means for energy while you are continuing to lightly exercise. Effectively cooling down also is thought to better facilitate a return to normal body temperature and to dampen nervous-system activity, which should promote better sleep at night.
What the Science Says:
When compared to passive recovery (laying horizontally for a similar amount of time), athletes who undertook active recovery post-exhaustive exercise not only outperformed the passive control group in sprint-fatigue testing 48 hours after initial exercise, but they also complained of less subjective soreness 24 and 48 hours post-initial exercise (31).
Research also stresses the importance of the recovery period being no more than 40% of VO2max, which may only be walking (32). Cooling down any harder has too high an energetic cost to be effective.
What This Means:
Although the mechanisms are not fully understood, it appears that active recovery is a relatively effective–and completely free–recovery tool. This might not always work for the time-crunched athlete, though, as science strongly suggests 10 to 20 minutes of very easy exercise post-regular workout (32).
Other Recovery Basics
Among all the gadgetry and trends, it might be easy to overlook our most accessible recovery tools of refueling, rehydration, and sleep.
There’s some current debate in the scientific literature about the window of proper fueling post-exercise, but we know that because our body is more insensitive to insulin after exercising, we can absorb carbohydrates more easily then. Additionally, there is evidence that GLUT4 (that glucose transporter we talked about in my article about ultramarathon eating) is more active post-exercise, which helps transport incoming carbohydrates through your small intestine. It’s because of this that we’re told to refuel during a perfectly ideal–and maybe slightly stressful–window of 30 to 60 minutes post-exercise. Is this 100% necessary after every single workout? Probably not, but if you are planning on training again later that same day or you did a particularly long or hard workout, glycogen re-synthesis becomes more important.
General refueling recommendations are to ingest approximately 1.1 to 1.5 grams of carbohydrates per 2.2 pounds (one kilogram) of body weight. For example, I weigh about 130 pounds (59 kilograms), so for me that’s 65 to 88 grams of carbohydrates (32).
Post-exercise rehydration is important because of your body’s desire to return to a state of homeostasis. When you are dehydrated post-exercise, and we all are to some degree, your body has to metabolically work to restore this balance on top of everything else it’s doing to recover from your workout. Dehydration also impairs other recovery functions. As we also learned in my ultra-eating article, dehydration impairs blood flow to your gut, making it nearly impossible to transport essential fuel through the small intestine’s walls. Dehydration also decreases your body’s total blood volume, and if recovery seems to hinge on adequate blood flow, you are on your back foot with dehydration-induced blood-volume loss. Effectively hydrate throughout your run and once you’ve finished so that recovery can proceed unimpaired (33).

Figure 12. The proper means of rehydrating post-exercise. Image: Ylmsportscience.com/2017/01/31/optimizing-post-exercise-rehydration/
Finally, sleep is important. If you want to know why, go read my article about it! Basically, when you don’t sleep enough, your body falls into a dysfunctional hormone cycle and this can leave you feeling fatigued and more prone to injury and chronic infection. Set yourself up first with this easy recovery modality.
The Takeaways
Amongst this wish list of recovery toys and a constantly evolving scientific understanding of their effectiveness, what’s a runner to do? Here are a few tips to help you navigate the muddy trails of exercise-recovery modalities:
- Proceed with caution: The research is a mixed bag at best when it comes to most recovery modalities and the market survives on their bioplausible nature. Remember that most of the positive research results so far come down to recovery tools making people feel better. While this is not a bad metric, it’s highly individual and weighted heavily in the psychological component of taking care of yourself. As we discussed, this is largely due to the fact that it’s really hard to create a blinded study to test for a placebo effect, so there could also be hidden but impactful variables at play.
- Be vigilant: Be an informed athlete, read the research, and be skeptical of product marketing that has no science basis. Also know that science in this field is emergent and our understanding of recovery tools will continue to evolve.
- Do what makes you feel good: With most of these nifty recovery tricks boiling down to working to relieve pain by hypothetically similar mechanisms and their effects based on subjective feelings, you might as well choose the options that make you and your training feel the best.
- Use your time and money wisely: Again, if we are working with largely subjective results, choose modalities that are cheap and take the least amount of time.
- Fatigue and inflammation from training are not all bad: Adequate stress plus adequate rest equals positive adaptation. Some level of inflammatory response is critical for the optimal repair of tissues damaged during the stress of training.
Call for Comments (from Meghan)
- What recovery modalities do you intentionally or unintentionally use to recover from running?
- Can you say if any of them subjectively feel good for you?
References
- Friel, J. (2017, April 10). Training: Stress, Fatigue, Recovery, Adaptation. Retrieved from https://www.joefrielsblog.com/2017/04/training-stress-fatigue-recovery-adaptation-1.html
- Dupuy, O., Douzi, W., Theurot, D., Bosquet, L., & Dugué, B. (2018). An Evidence-Based Approach for Choosing Post-exercise Recovery Techniques to Reduce Markers of Muscle Damage, Soreness, Fatigue, and Inflammation: A Systematic Review With Meta-Analysis. Frontiers in Physiology,9. doi:10.3389/fphys.2018.00403
- Hausswirth, C., Louis, J., Bieuzen, F., Pournot, H., Fournier, J., Filliard, J., & Brisswalter, J. (2011). Effects of Whole-Body Cryotherapy vs. Far-Infrared vs. Passive Modalities on Recovery from Exercise-Induced Muscle Damage in Highly-Trained Runners. PLoS ONE,6(12). doi:10.1371/journal.pone.0027749
- Bender, P. U., Luz, C. M., Feldkircher, J. M., & Nunes, G. S. (2019). Massage therapy slightly decreased pain intensity after habitual running, but had no effect on fatigue, mood or physical performance: A randomised trial. Journal of Physiotherapy,65(2), 75-80. doi:10.1016/j.jphys.2019.02.006
- V. Morhenn, L.E. Beavin, P.J. ZakMassage increases oxytocin and reduces adrenocorticotropin hormone in humans. Alternative Therapy Health Medicine, 18 (2012), pp. 11-18
- Field, M. Hernandez-Reif, M. Diego, S. Schanberg, C. KuhnCortisol decreases and serotonin and dopamine increase following massage therapy. International Journal Neuroscience, 115 (2005), pp. 1397-1413
- Cochrane, D., Booker, H., Mundel, T., & Barnes, M. (2013). Does Intermittent Pneumatic Leg Compression Enhance Muscle Recovery after Strenuous Eccentric Exercise? International Journal of Sports Medicine,34(11), 969-974. doi:10.1055/s-0033-1337944
- Heapy, A. M., Hoffman, M. D., Verhagen, H. H., Thompson, S. W., Dhamija, P., Sandford, F. J., & Cooper, M. C. (2018). A randomized controlled trial of manual therapy and pneumatic compression for recovery from prolonged running – an extended study. Research in Sports Medicine,26(3), 354-364. doi:10.1080/15438627.2018.1447469
- Cochrane, D., Booker, H., Mundel, T., & Barnes, M. (2013). Does Intermittent Pneumatic Leg Compression Enhance Muscle Recovery after Strenuous Eccentric Exercise? International Journal of Sports Medicine,34(11), 969-974. doi:10.1055/s-0033-1337944
- Poppendieck, W., Wegmann, M., Ferrauti, A., Kellmann, M., Pfeiffer, M., & Meyer, T. (2016). Massage and performance recovery: A meta-analytical review. Sports Medicine, 46, 183–
- Kraemer, W. J., Bush, J. A., Wickham, R. B., Denegar, C. R., Gomez, A. L., Gotshalk, L. A., et al. (2001). Continuous compression as an effective therapeutic intervention in treating eccentric-exercise-induced muscle soreness. J. Sport Rehabil. 10, 11–23. doi: 10.1123/jsr.10.1.11
- Wiewelhove, T., Döweling, A., Schneider, C., Hottenrott, L., Meyer, T., Kellmann, M., . . . Ferrauti, A. (2019). A Meta-Analysis of the Effects of Foam Rolling on Performance and Recovery.Frontiers in Physiology,10. doi:10.3389/fphys.2019.00376
- Babault, N., Cometti, C., Maffiuletti, N. A., & Deley, G. (2011). Does electrical stimulation enhance post-exercise performance recovery?European Journal of Applied Physiology,111(10), 2501-2507. doi:10.1007/s00421-011-2117-7
- Borne, R., Hausswirth, C., & Bieuzen, F. (2017). Relationship Between Blood Flow and Performance Recovery: A Randomized, Placebo-Controlled Study.International Journal of Sports Physiology and Performance,12(2), 152-160. doi:10.1123/ijspp.2015-0779
- Stein, K. (2018, December 11). Recovery Modalities: An Update on the Science. Retrieved from https://pbats.com/recovery-modalities/
- Halson, S. (2013). Recovery techniques for athletes. Sports Science Exchange. Vol. 26, No. 120, 1-6. www.gssiweb.org
- Neric FB, Beam WC, Brown LE, Wiersma LD (2009) Comparison of swim recovery and muscle stimulation on lactate removal after sprint swimming. J Strength Cond Res 23:2560–2567
- Halson, S. L., Bartram, J., West, N., Stephens, J., Argus, C. K., Driller, M. W., . . . Martin, D. T. (2014). Does Hydrotherapy Help or Hinder Adaptation to Training in Competitive Cyclists?Medicine & Science in Sports & Exercise,46(8), 1631-1639. doi:10.1249/mss.0000000000000268
- Leeder, J., Gissane, C., Someren, K. V., Gregson, W., & Howatson, G. (2011). Cold water immersion and recovery from strenuous exercise: A meta-analysis.British Journal of Sports Medicine,46(4), 233-240. doi:10.1136/bjsports-2011-090061
- Wilson, L. J., Dimitriou, L., Hills, F. A., Gondek, M. B., & Cockburn, E. (2018). Whole body cryotherapy, cold water immersion, or a placebo following resistance exercise: A case of mind over matter?European Journal of Applied Physiology,119(1), 135-147. doi:10.1007/s00421-018-4008-7
- Hausswirth, C., Louis, J., Bieuzen, F., Pournot, H., Fournier, J., Filliard, J., & Brisswalter, J. (2011). Effects of Whole-Body Cryotherapy vs. Far-Infrared vs. Passive Modalities on Recovery from Exercise-Induced Muscle Damage in Highly-Trained Runners.PLoS ONE,6(12). doi:10.1371/journal.pone.0027749
- Rose, C., Edwards, K., Siegler, J., Graham, K., & Caillaud, C. (2017). Whole-body Cryotherapy as a Recovery Technique after Exercise: A Review of the Literature.International Journal of Sports Medicine,38(14), 1049-1060. doi:10.1055/s-0043-114861
- Krueger, M., Costello, J. T., Achtzehn, S., Dittmar, K., & Mester, J. (2019). Whole-body cryotherapy (−110 °C) following high-intensity intermittent exercise does not alter hormonal, inflammatory or muscle damage biomarkers in trained males.Cytokine,113, 277-284. doi:10.1016/j.cyto.2018.07.018
- Fonda B, Sarabon N. E ects of whole-body cryotherapy on recovery after hamstring damaging exercise: A crossover study. Scand J Med Sci Sports 2013; 23: e270–e278
- Ziemann E, Olek RA, Grzywacz T, Kaczor JJ, Antosiewicz J, Skrobot W, Kujach S, Laskowski R. Whole-body cryostimulation as an e ective way of reducing exercise-induced in ammation and blood cholesterol in young men. Eur Cytokine Netw 2014; 25: 14–23
- Morhenn, V., Beavin, L., & Zak, P. (2012). Massage increases oxytocin and reduces adrenocorticotropin hormone in humans.Alternative Therapy Health and Medicine,18(6), 11-18.
- Hill, Jessica, Howatson, Glyn, van Someren, Ken, Gaze, David, Legg, Hayley, Lineham, Jack and Pedlar, Charles (2016) The effects of compression garment pressure on recovery from strenuous exercise. International Journal of Sports Physiology and Performance. ISSN 1555-0265 (In Press)
- Lim, C. S., & Davies, A. H. (2014). Graduated compression stockings.Canadian Medical Association Journal,186(10). doi:10.1503/cmaj.131281
- Machado, A. F., Ferreira, P. H., Micheletti, J. K., Almeida, A. C., Lemes, Í R., Vanderlei, F. M., . . . Pastre, C. M. (2015). Can Water Temperature and Immersion Time Influence the Effect of Cold Water Immersion on Muscle Soreness? A Systematic Review and Meta-Analysis.Sports Medicine,46(4), 503-514. doi:10.1007/s40279-015-0431-7
- Higgins, T. R., Greene, D. A., & Baker, M. K. (2017). Effects of Cold Water Immersion and Contrast Water Therapy for Recovery From Team Sport.Journal of Strength and Conditioning Research,31(5), 1443-1460. doi:10.1519/jsc.0000000000001559
- Reilly, T., & Ekblom, B. (2005). The use of recovery methods post‐Journal of Sports Sciences,23(6), 619-627. doi:10.1080/02640410400021302
- Mika, A., Oleksy, Ł, Kielnar, R., Wodka-Natkaniec, E., Twardowska, M., Kamiński, K., & Małek, Z. (2016). Comparison of Two Different Modes of Active Recovery on Muscles Performance after Fatiguing Exercise in Mountain Canoeist and Football Players.Plos One,11(10). doi:10.1371/journal.pone.0164216
- Evans, G. H., James, L. J., Shirreffs, S. M., & Maughan, R. J. (2017). Optimizing the restoration and maintenance of fluid balance after exercise-induced dehydration.Journal of Applied Physiology,122(4), 945-951. doi:10.1152/japplphysiol.00745.2016


