Welcome to Running on Science’s second edition of mythbusting! Once again, I’ve returned from the trailheads, run clubs, and dark parts of the internet to examine four more topics I hear trail runners and ultrarunners talking about. In this article, we will use current scientific understanding to decide if these tidbits are fact, fiction, or something in-between.
Fact or Fiction: “Shoes with more cushioning prevent injury.”
Let’s talk about the ‘battle’ of maximal versus all other shoes–both minimal and conventional–and how they affect a runner’s likelihood of injury. Over the past two decades, we have seen massive swings in shoe-industry trends from traditional shoes to the barefoot movement and subsequently minimal shoes, and then to the next extreme of maximal shoes. While minimal shoes have been defined by both their lack of cushioning and heel-to-toe drop, there remains no set academic definition of maximal shoes (12). So, we simply say that maximal shoes contain “extreme” additional cushioning, specifically in the midsole, with the implied intent of reducing impact force during running (1, 12).
To start, 40% of runners are expected to experience a running-related injury this year and, generally speaking, those injuries typically result from the repeated overloading of muscles, bones, ligaments, tendons, and joints (2). Depending on a number of factors, including how fast you run and your biomechanics, the force applied to your joints when running can be five to 12 times your bodyweight (3). These facts might make us think that extra cushioning could reduce the ‘blow’ of every step and make us less injury prone.
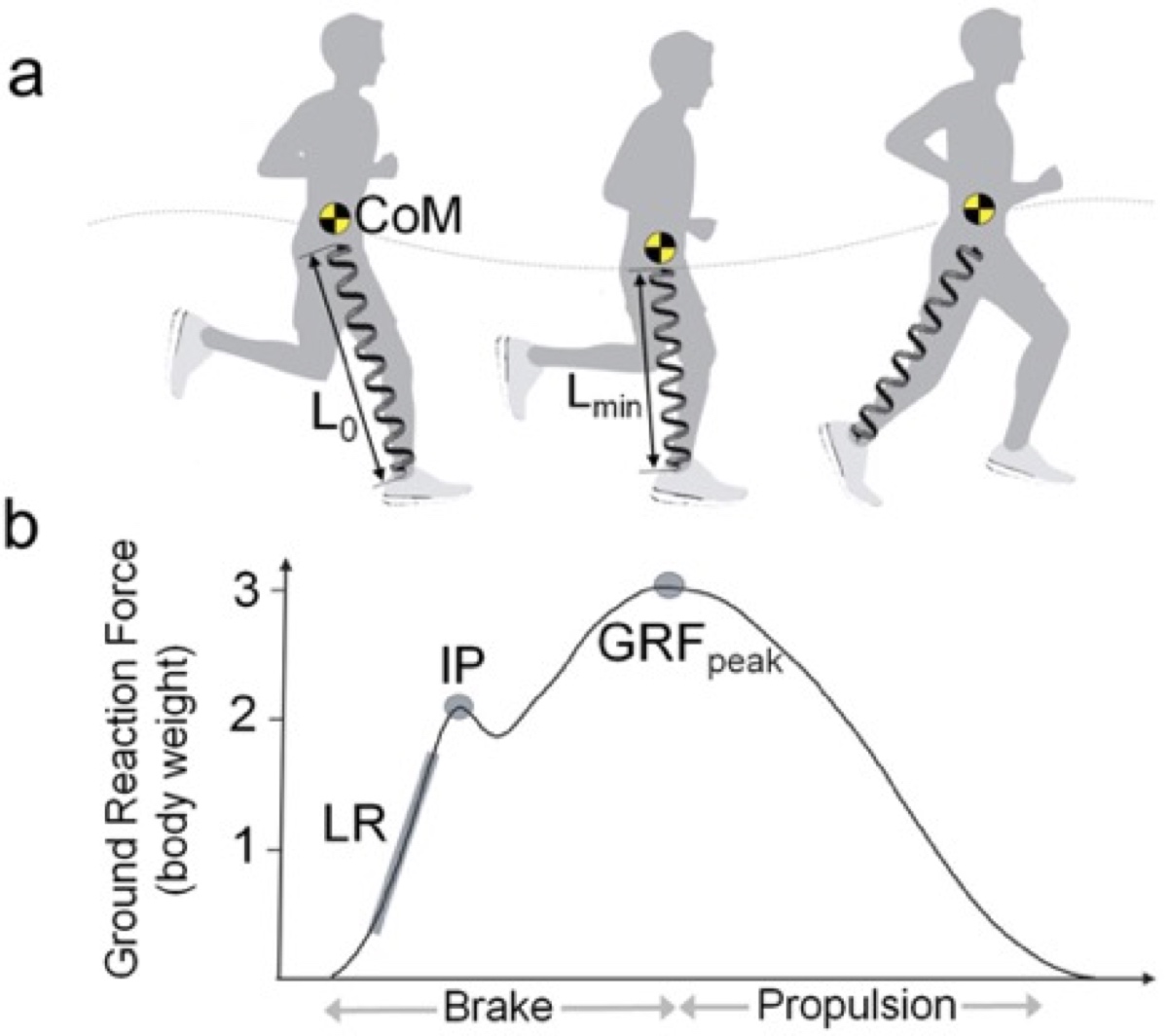
A graphic showing how the body impacts the ground and is loaded with ground reaction force during running. In the B portion of the graphic, LR stands for loading rate, IP stands for impact peak, and GRFpeak stands for peak ground reaction force. In the A portion of the graphic: L0 stands for the initial leg-spring length, Lmin stands for the minimal leg-spring length, and CoM stands for the body’s center of mass. Image: Kulmala, Juha-Pekka, et al. “Running in Highly Cushioned Shoes Increases Leg Stiffness and Amplifies Impact Loading.” Scientific Reports, vol. 8, no. 1, 2018, doi:10.1038/s41598-018-35980-6. Retrieved from: Nature.com/articles/s41598-018-35980-6?fbclid=IwAR1t6YbnuSCaOM6QmHzC0xhhOu_x-ydB0hWJbqWBEGMkbeNJQFQIlm9j6Zc
But that’s not true, and the reasons why are truly fascinating. Over the past decade and despite running-shoe-industry swings among traditional, minimal, and maximal shoes as well as other changes in shoe technology, the chance of sustaining a running-related injury has remained relatively stable (12).
It turns out that we change our running mechanics slightly when we run in maximal shoes versus conventional shoes and this slight change matters. A study found that maximal shoes actually amplify instead of attenuate peak impact force (the force exerted by the ground on the body) and loading rate (the speed at which force impacts the body), independent of how fast you run (2). We currently theorize that in a maximal shoe, similar to when you transition from running on a firm surface to a soft one, you stiffen your leg more to control your center of mass and by doing so your leg physically compresses less. Essentially, your body mechanically counters all that soft cushioning which magnifies impact force (2).
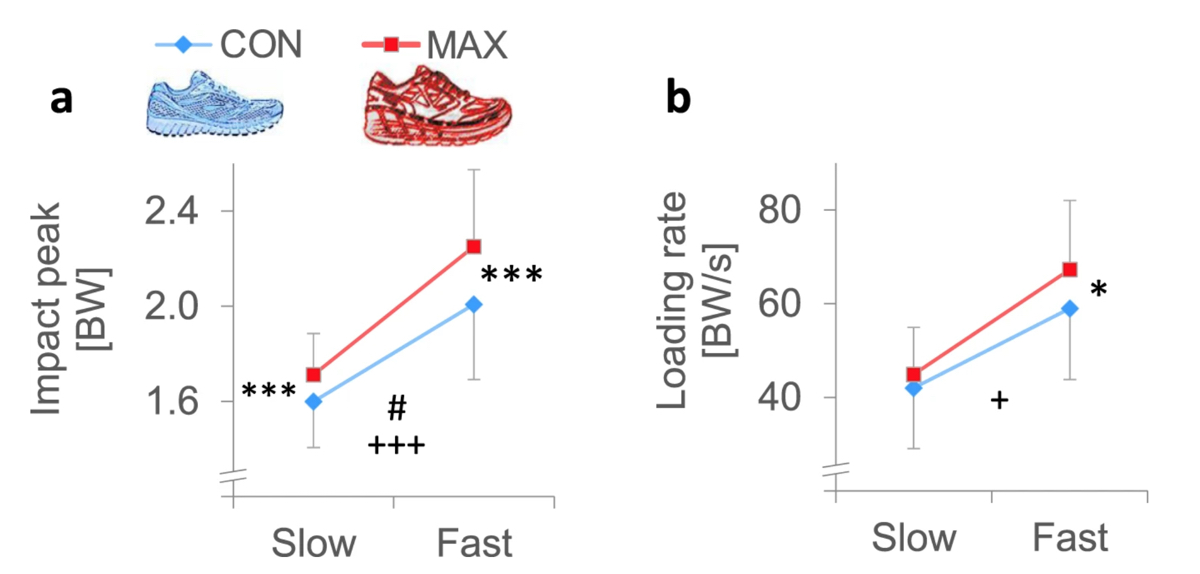
A graphic showing the results of a study which demonstrated that, independent of how fast an individual was running (10 kilometers/hour versus 14.5), in maximal shoes (Hoka Conquest, heel height 43.9 millimeters, forefoot height 38.5mm) the impact peak (force exerted by the ground on the body) and loading rate (speed at which force is applied to the body) were higher than when running in more conventional shoes (Brooks Ghost, heel height 35.6mm, forefoot height 22.9mm). Image: Nature.com/articles/s41598-018-35980-6?fbclid=IwAR1t6YbnuSCaOM6QmHzC0xhhOu_x-ydB0hWJbqWBEGMkbeNJQFQIlm9j6Zc
Maybe you just need to get used to your maximal shoes? That answer is also no, but with some caveats. In a study, runners were given six weeks to adjust to a maximal shoe. Over those six weeks, there was a negligible change in impact force and loading rate in the maximal shoes and the impact force and loading rate were still greater in maximal shoes as compared to conventional shoes. Interestingly, this study suggested that the extended duration of eversion (a component of pronation specific to the ankle) when running in maximal shoes might cause some injuries sustained in them (4). Runners who have prolonged eversion duration often also have more incidences of Achilles tendinopathy and medial tibia stress syndrome (shin splints), and possibly bone-stress injuries of the tibia (4).

A photo taken during a research project (2) which determined that even with an adjustment period, impact forces and loading rates were still greater in runners wearing maximal shoes as compared to conventional shoes. Image: Today.oregonstate.edu/news/despite-transition-period-maximal-running-shoes-may-still-lead-increased-risk-injury
Conclusion
Fiction–at least for now, since this is a burgeoning research field. If you are using a maximal shoe to rid yourself of or avoid injury, you’re better off addressing the underlying reasons for what ails you. Essentially, the science has shown so far that cushioned shoes don’t protect you from poor biomechanics. Further, if you are prone to ankle, Achilles, and tibia issues, then research has so far shown that maximal shoes might do more harm than good.
Fact or Fiction: “NSAIDs enhance performance.”
This tidbit really piqued my interest. Truthfully, I’m wary of in-race NSAIDs, or non-steroidal anti-inflammatory drugs, like ibuprofen and aspirin because research shows this leads to an increased risk of gastrointestinal issues and kidney injury. But I have not previously shied away from them due to sports ethos. I got to digging, and I’ll tell you, it’s interesting! By the way, you can read more about kidneys and NSAIDs as well as gastrointestinal issues and NSAIDs elsewhere on iRunFar.
NSAIDs are the most common pharmacological substances used by athletes (5, 6). Generally, athletes use them to run through minor injuries and niggles because they relieve pain and reduce inflammation. In fact, athletes are four times more likely to use a medication like NSAIDs prophylactically (pre-treating an injury) than a recreational exerciser.
While we know a lot about how NSAIDs can be and are used to treat sports injuries, there’s a lot less literature on their pharmacological action related to performance enhancement. NSAIDs work by inhibiting the activity of cyclooxygenase oxidases (COX, a family of enzymes that produce an active compound that promotes inflammation, pain, and fever) (5). By blocking the COX enzymes, NSAIDs mask their nociceptive effect (a sensory nervous system reaction to pain or damage in the body). In theory, with these masked, you can ‘push through pain.’ However, most research–albeit almost exclusively done in the strength and conditioning world–has been inconclusive.
What about a close cousin to NSAIDs, specifically paracetamol, what’s also known as acetaminophen. This is another incredibly common over-the-counter analgesic used primarily for minor aches and pains as well as a fever reducer.
The exact mechanism of acetaminophen’s painkilling effects is not fully understood, but it’s believed that acetaminophen targets the channels in the primary sensory neurons by directly inhibiting their signals (working directly on the brain and spinal cord’s perception of pain) (5). Additionally, it’s been suggested that acetaminophen might be able to directly affect the CB1 receptor (a cannabinoid receptor, the same one that tetrahydrocannabinol [THC] binds to) in the brain or spinal cord, thereby influencing the cognitive processing of pain (5).
Unlike with NSAIDs, we have some endurance-focused performance data with therapeutic doses, including a 5% increase in power output, reduced time required to complete a cycling time trial, and increased time to exhaustion in cyclists (5). Another significant difference in the two medications is that limited negative side effects during endurance exercise exist with acetaminophen at therapeutic doses. However, toxicity does exist at five to 10 grams/day (which is well above the therapeutic dose) and puts you at risk for liver damage particularly if combined with alcohol as your liver has to metabolize both. What’s really interesting, and specific to the ultra community, is acetaminophen’s role as a fever reducer. There is new research coming out in this area, but for now we would recommend against using it during hot races as it has potential to leave you misreading the thermal stress your body is under (5).”
Since we’re talking about performance enhancement in sports, we should note that NSAIDs and acetaminophen are not on the World Anti-Doping Agency banned list. However, races now partnered with Quartz including the Golden Trail Series for 2020 state that racers should not ingest NSAIDs 24 hours prior to the event. How this is possibly enforced is a head scratcher, but it will be interesting to watch nonetheless.
Conclusion
It’s a draw! NSAIDs are under-researched from a performance standpoint in endurance sports, but the lengthy list of negative side effects likely outweighs any modest performance improvement when administered prophylactically. On the other hand, there might be something to a low therapeutic dose of acetaminophen in endurance sports for the purpose of legally aiding performance.
Fact or Fiction: “You could hurt your baby if you run while pregnant.”
Can we just outright say, fiction! While the scientific literature so far shows that running while pregnant won’t harm a baby and will lead to a number of health benefits, I’ve still overheard my fair share of skepticism. Can we blame the public for being so woefully ignorant? Women weren’t even allowed to do races longer than 200 meters until the 1960 Olympics because they were deemed too frail. It took until 1980 for the American College of Sports Medicine to come out in defense of women with a consensus statement advocating for women in competitive running. I would like to continue this rant about historic sexist decisions made about female athletes which had no scientific basis and the continued underrepresentation of women in exercise-science research, but I’ll save that for another day.
So, what do we know about running for two? We know that fetal health during exercise is under-researched, and that’s largely due to the inherent risk of pregnant women and their babies as test subjects. However, pregnant women do exercise and women who exercise also happen to get pregnant, so it’s important to understand what the actual risks are if medical professionals are going to confidently–and correctly–advise their pregnant patients. In fact, until recently many doctors still recommended pregnant women keep their heart rates below 140 beats per minute during exercise, despite the fact that this recommendation was removed from the American College of Obstetricians and Gynecologists guidelines in 1994 (8)!
Some of the concerns of exercising while pregnant have been the worry of diminished blood flow to the uterus (because your working muscles need more blood), exercise-generated heat stress for the mother and child (since your core body temperature naturally rises when you exercise), preterm delivery (if running were to impact the cervix’s integrity), and abnormal maternal and fetal heart rates (7). However, research shows that moderate (55 to 69% of maximum heart rate) to vigorous (70 to 89% of maximum) activity while pregnant does not change placental blood circulation or show signs of fetal stress even at 36 to 37 weeks of gestation (8). The human body is not only good at keeping us alive but keeping a whole other tiny human alive as well.
But what about the jostling? While not every woman will feel comfortable running while pregnant, the physical act of running (and that pesky ground reaction force) will not hurt baby-to-be. Wee ones fly first class in the coziest sac of amniotic fluid a woman’s body can make. What I mean to say is, daily abdominal contact, jostling, and the impacts of activities like running have very little affect on a baby that is protected by both the muscular organ that is the uterus and the literal shock absorber that is amniotic fluid.
In fact, exercising while pregnant has a lot of positive benefits for both mom and baby, which include a decreased risk of gestational diabetes, hypertension, pre-eclampsia, and postpartum weight retention (7, 8). To learn more, check out iRunFar’s in-depth article on the science of running while pregnant.
Conclusion
Fiction! While not all women will be able to run to full term–put a bowling ball in your shirt and see how it feels–the literature shows that running itself, even fairly intense running, will not harm their babies. However, every woman is different, so consult with your healthcare provider before starting or changing your exercise program.
Fact or Fiction: “Increase your weekly volume by no more than 10% each week to avoid injury.”
We’ve all heard that by using the ‘10% rule,’ or the rule of thumb by which we slowly increase our running volume over time, we’ll avoid injury. An example of following this rule would be to run 20 miles one week one, 22 miles on week two, 24.2 miles on week three, and so forth. Is this a hard-and-fast rule, or is it more of a rule of thumb? What does it mean for experienced versus brand-new runners? As a scientist, self-proclaimed ultra nerd, and endurance coach, should I consider this a ‘foundational concept’ or one of the many tools in my toolshed?
A massive research project is currently underway, following 20,000 runners for 18 months, and looking at training-volume changes and running-related injuries. It’s a very exciting project which will add to our understanding on this topic, but until they’ve collected and crunched all the numbers, we will have to look at research that is a little older and primarily done with novice runners (13).
In 2007, a research group studied 532 runners training for a four-mile race. One group was placed in an eight-week program running three days a week with an approximate volume increase of 23% per week, and a second group was placed on a more conservative 13-week program running three days a week with an approximate volume increase of 10% per week. When it was all said and done, one in five runners in both groups experienced a running-related injury (9).
Maybe they needed more conditioning before they started running, since they were novice runners? Researchers ran the study again, this time randomly assigning one group an additional four-week program of walking, hopping, and jumping rope before they started an identical 13-week program. Once again, they saw that one in five participants suffered from a running-related injury (9, 11).
There is one more study of interest, one that followed 873 runners for one year where approximately 23% of the runners experienced a running-related injury (10). In this study, a connection between volume increases in the two weeks prior to injury was identified amongst runners. Runners who increased their mileage by more than 30% over two weeks were much more likely to sustain an injury than those who increased their mileage by less than 10% (10). They also found that runners who made this rapid jump were at much higher risk for specific injuries such as patellofemoral pain (runner’s knee), ilotibial band syndrome, patellar tendonopathy, and gluteus medius tendinitis and associated greater trochanteric bursitis (hip pain). But maybe the most interesting thing of all was that plantar fasciitis, Achilles tendinopathy, calf injuries, hamstring injuries, tibial stress fractures, and hip flexor strains were found within the group following the 10% rule, suggesting these injuries are related to something other than training volume (10).
Conclusion
It’s a draw! A wise person once said, “We don’t know what we don’t know yet,” and this is true for the 10% rule. Research on this is in progress, and perhaps this under-researched area will continue to get more attention in the future. In the meantime, while the 10% rule might be a conservative option, it’s clear that it’s neither the only option nor a guarantee that you won’t get injured. What does appear to be true is that some specific injuries are linked to a dramatic increase in volume more than others. So if you have some screaming iliotibial-band pain or a cranky hip or knee, it might just be worth keeping your volume in check. And remember, training is not always a linear process!
Call for Comments (from Meghan)
- Alright, let’s talk about these facts and fictions! Have you followed or broken the ‘10% rule’ over the years? What anecdotes can you share about it?
- How about maximal shoes? Have you used them with the intent of trying to avoid or address injury?
- NSAIDs and acetaminophen, do you use them in your training and racing and if so have you found them to help you perform?
- Mother runners, care to share your story of running or not running while pregnant?
References
- Mercer, M. A., Stone, T. M., Young, J. C., Mercer, J. (2018). Running Economy while Running in Extreme Cushioning and Normal Cushioning Running Shoes. International Journal of Exercise Science, 11(2), 1031-1040
- Kulmala, Juha-Pekka, et al. “Running in Highly Cushioned Shoes Increases Leg Stiffness and Amplifies Impact Loading.” Scientific Reports, vol. 8, no. 1, 2018, doi:10.1038/s41598-018-35980-6.
- Kenneth P. Clark, Laurence J. Ryan, Peter G. Weyand. A general relationship links gait mechanics and running ground reaction forces. The Journal of Experimental Biology, 2017; 220 (2): 247 DOI: 10.1242/jeb.138057
- Hannigan, J.j., and Christine D. Pollard. “Differences in Running Biomechanics between a Maximal, Traditional, and Minimal Running Shoe.” Journal of Science and Medicine in Sport, vol. 23, no. 1, 2020, pp. 15–19., doi:10.1016/j.jsams.2019.08.008.
- Holgado, D., Sanabria, D., Hopker, J. “Analgesics and Sport Performance: Beyond the Pain-Modulating Effects.” PM&R, vol. 10, no. 1, Apr. 2017, pp. 72–82., doi:10.1016/j.pmrj.2017.07.068.
- André, C., Girard, J., Gautier, S., Derambure, P., Rochoy, M. “Training Modalities and Self-Medication Behaviors in a Sample of Runners during an Ultratrail.” Science & Sports, vol. 35, no. 1, 2020, doi:10.1016/j.scispo.2019.04.007.
- Kuhrt, Katy, et al. “Is Recreational Running Associated with Earlier Delivery and Lower Birth Weight in Women Who Continue to Run during Pregnancy? An International Retrospective Cohort Study of Running Habits of 1293 Female Runners during Pregnancy.” BMJ Open Sport & Exercise Medicine, vol. 4, no. 1, 2018, doi:10.1136/bmjsem-2017-000296.
- Szymanski, Linda M, and Andrew J Satin. “Exercise During Pregnancy: Fetal Responses to Current Public Health Guidelines.” Obstet Gynecol., vol. 119, no. 3, Mar. 2012, pp. 603–610., doi:10.1097/AOG.0b013e31824760b5.
- Buist, Ida, et al. “The GRONORUN Study: Is a Graded Training Program for Novice Runners Effective in Preventing Running Related Injuries? Design of a Randomized Controlled Trial.” BMC Musculoskeletal Disorders, vol. 8, no. 1, Feb. 2007, doi:10.1186/1471-2474-8-24.
- “Running: How to Safely Increase Your Mileage.” Journal of Orthopaedic & Sports Physical Therapy, vol. 44, no. 10, 2014, pp. 748–748., doi:10.2519/jospt.2014.0506.
- Nielsen, R., Buist, I., Sørensen, H., Lind, M., Rasmussen, S. Training Errors and Running Related Injures: a Systematic review. Int J Sports Phys Ther. Vol. 7, no. 1, Feb. 2012, pp. 58-75., doi:
- Pollard, Christine D., et al. “Influence of Maximal Running Shoes on Biomechanics Before and After a 5K Run.” Orthopaedic Journal of Sports Medicine, vol. 6, no. 6, 2018, p. 232596711877572., doi:10.1177/2325967118775720.
- Nielsen, Rasmus Østergaard, et al. “The Garmin-RUNSAFE Running Health Study on the Aetiology of Running-Related Injuries: Rationale and Design of an 18-Month Prospective Cohort Study Including Runners Worldwide.”BMJ Open, vol. 9, no. 9, 2019, doi:10.1136/bmjopen-2019-032627.