With this article, I aim to provide runners with a resource about the acute effects of racing on the heart and the long-term effects of running (or regular cardiovascular exercise) on the heart and on our health. The long-term effects of running on the heart and on health in general are overall very beneficial. Specific cardiac changes can occur in endurance athletes, which runners should be aware of. In very rare and specific circumstances—which are outlined in this article—running can result in collapse or death due to problems with the heart.
Introduction
It was an exceptionally warm and humid day on the coast of Denmark. A physician friend and I were running a point-to-point marathon, mostly together, both pushing it. It was the kind of day where a breeze would have been delightful, but there was a tailwind the entire way. Normally, this would be helpful, but it felt like my sweat was just not evaporating. The two of us crossed the finish line within minutes of each other—both ecstatic to be done—hugged, and looked forward to the post-race festivities. But then, a couple minutes behind us, a middle-aged man came sprinting across the finish line against another runner, clutched his chest, and then collapsed.
We both ran to him, knowing via our medical training that a person who collapses while running has had a cardiac arrest until proven otherwise. And he was pulseless. “Get a defibrillator! Call an ambulance!” one of us yelled. Other bystanders joined in to help. My friend ran the resuscitation–she was an emergency-medicine doctor and I was an ophthalmologist—so she took the lead. After a few rounds of cardiopulmonary resuscitation (CPR) and a couple shocks, we revived him. His wife erupted in tears of joy and the ambulance arrived to take him to the nearest hospital. We all looked at each other, relieved. How fortunate the race had a defibrillator ready, just in case. We never did learn the cause of his cardiac arrest, but given his age, coronary-artery disease was the most likely cause. (More on this to come, so read on.)
I think of this instance often when people ask me now, as an endurance-sports researcher and physical-medicine and rehabilitation doctor, if running is safe for the heart.
When people ask this question, I like to think that they are really asking two questions:
- What is the short-term risk of suffering a cardiac event (“heart attack” or dangerous cardiac rhythm) while running/racing?
- What are the long-term effects of running on the heart?
The answer to Question 1 is that there is, indeed, a slightly increased risk of a cardiac event during strenuous exercise, if you are predisposed (by coronary-artery disease, hypertrophic cardiomyopathy, and many other conditions, the most common of which are listed in Figure 5). However, this risk is overall very, very small. The answer to Question 2 is that running and exercise greatly improve cardiovascular health and decrease your cardiac risk and overall mortality.
Background on the Heart and Cardiac Problems
Cardiac arrest is when the heart stops pumping blood. Cardiac arrest can be caused by lack of blood flow to the heart itself (a “heart attack”), most often due to coronary-artery disease, or by a structural abnormality of the heart that causes it to suddenly start beating irregularly (an arrhythmia) and ineffectively. These are more likely to occur anytime the heart is working harder to pump blood, such as during exercise.
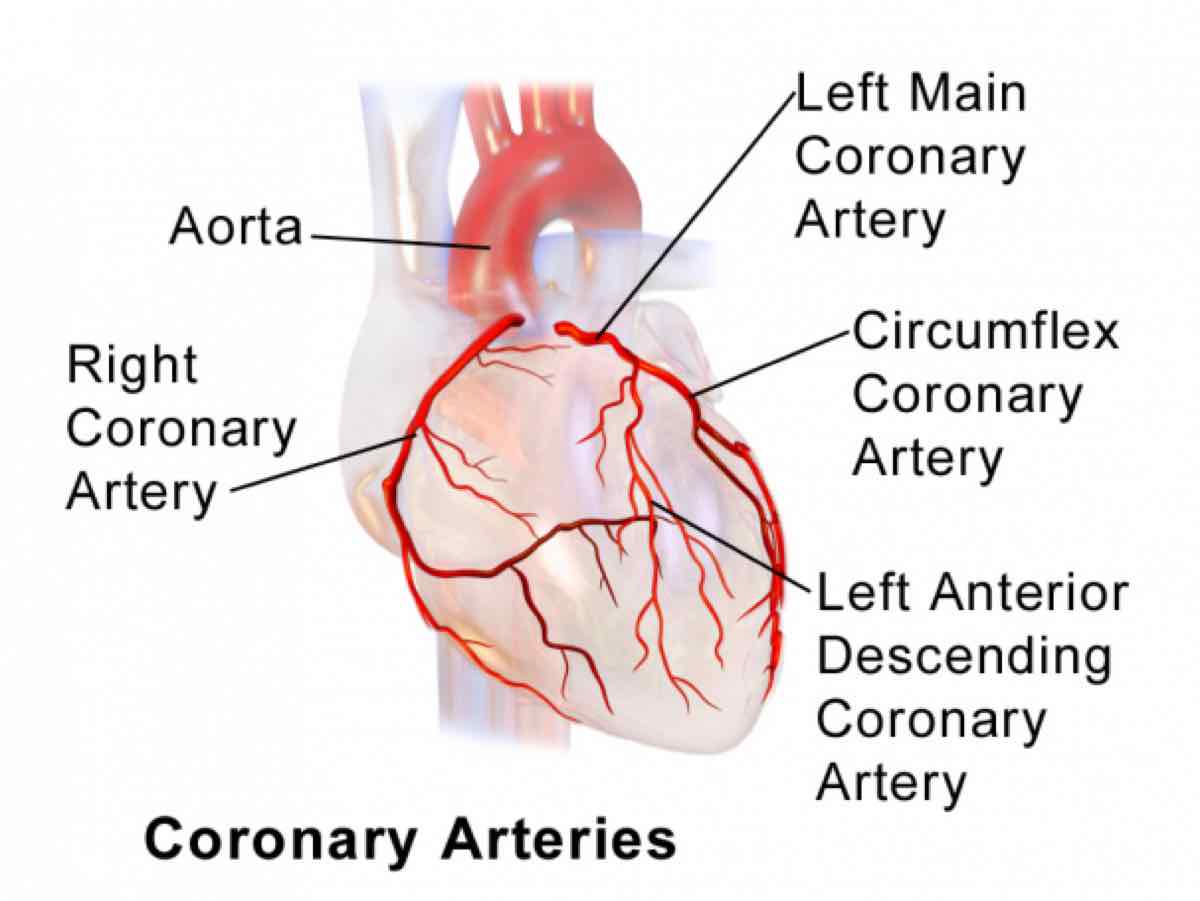
Figure 1. The outside of the heart. The heart gets its blood supply from the coronary arteries. When the heart does not get enough blood through these arteries, a person can experience a “heart attack” or myocardial ischemia. Heart attacks are the most common cause of sudden cardiac death in runners over 40. Image by the The Society of Thoracic Surgeons.
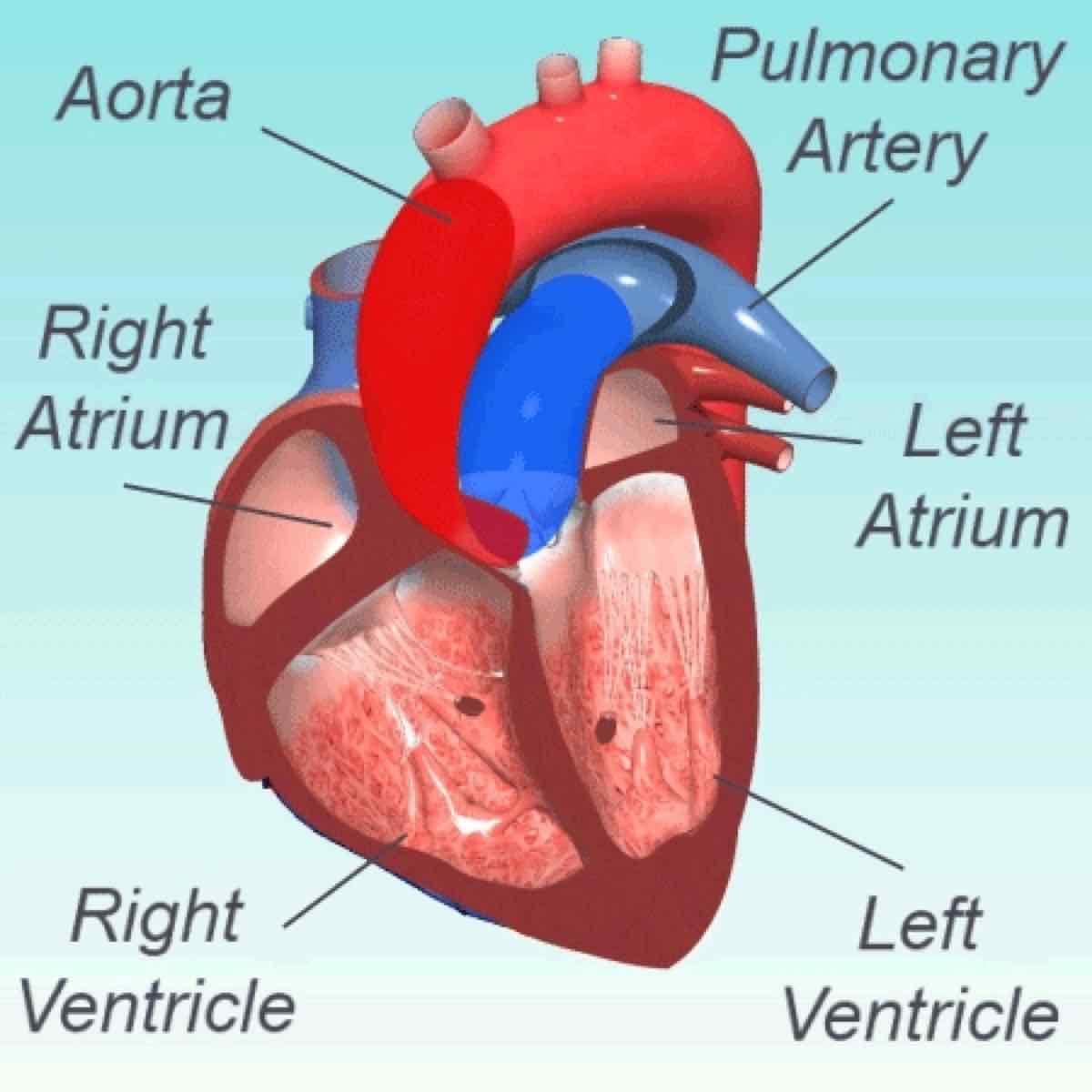
Figure 2. The inside of the heart. Alterations in the anatomy of the heart can interfere with the heart’s ability to beat regularly. When the heart beats irregularly, that is called an arrhythmia. Certain types of arrhythmias can cause sudden cardiac death. Image by The Society of Thoracic Surgeons.
Sudden cardiac death caused by either a “heart attack” or an arrhythmia can sometimes be reversed with CPR, especially if started quickly after the collapse and a defibrillator is present. CPR should always be attempted when a person collapses and is pulseless.
Epidemiology of Sudden Cardiac Death in Marathons and Ultramarathons
Fortunately, the risk of sudden cardiac death during a marathon is exceptionally low at 0.0008-0.001%, but higher than in a half marathon, which is 0.00027% (Kim, 2012; Redelmeier, 2007). Just to put this in perspective, this is the approximate equivalent risk of riding a motorcycle for two hours, cycling for 10 hours, or riding in a car for 28 hours (Redelmeier, 2007). And, in fact, due to street closures in big-city marathons, it is estimated that there is a 35% decrease in overall mortality due to marathons because of the prevention of motor vehicle accident deaths (Redelmeier, 2007).

Figure 3. Aerial photo of the New York City Marathon as runners cross the Verazzano Bridge. The marathon now has over 50,000 participants yearly. Photo: Metropolitan Transportation Authority of the State of New York
As for ultramarathons, I have found only a handful of cases of cardiac arrest reported. Two were at the Comrades Marathon in 2007 when two men collapsed with cardiac arrest near the finish line. One was resuscitated but died in the hospital; the other collapsed near the finish and was carried by runners across the finish line, apparently delaying medical attention, and that runner was not revived (Ross, 2007).
Perhaps a more interesting story is that of the relatively high prevalence of cardiac arrest at the Marathon des Sables. There have been at least four cardiac arrests of the approximately 20,000 total participants since the race’s inception. That is a rate of 0.02% (a 200-times increased rate compared with marathons of 0.0001%). The first reported cardiac arrest was in 1988 when a 29-year-old Frenchman collapsed on a sand dune and died of a heart attack on a day the temperature reached 56 degrees Celsius/132 degrees Fahrenheit (Roe, 2014). Then in 2007, one 49-year-old male competitor without known health problems died of a heart attack in his sleep after the longest, 50-mile-ish stage (Marathon des Sables Training Blog, accessed 2018). Third, in 2012, a male participant collapsed after telling his friends he did not feel well. He was successfully revived, but additional details are not known (Hicks, 2018). Finally, in 2017 a male runner of an unknown age had a cardiac arrest at a checkpoint and was successfully revived with CPR (Dewall, 2017). The 0.02% chance of cardiac arrest at Marathon des Sables is likely an underestimate, given there is no systematic reporting of these occurrences and begs the question of why this race seems to have an increased rate compared with marathons. (Clearly it is not only the length of the race as it is only about six times longer than a marathon.)

Figure 4. The Marathon des Sables is a 250-kilometer stage race across the Sahara Desert held every year in April, with high temperatures often reaching over 50 degrees Celsius. Photo: Cimbaly/Marathon des Sables
Causes of Sudden Cardiac Death During Exercise
The most likely causes of sudden cardiac death during exercise are dependent on the person’s age. In athletes under 40, it is typically a congenital condition (see Figure 5) and in runners over 40, it is most often coronary-artery disease.
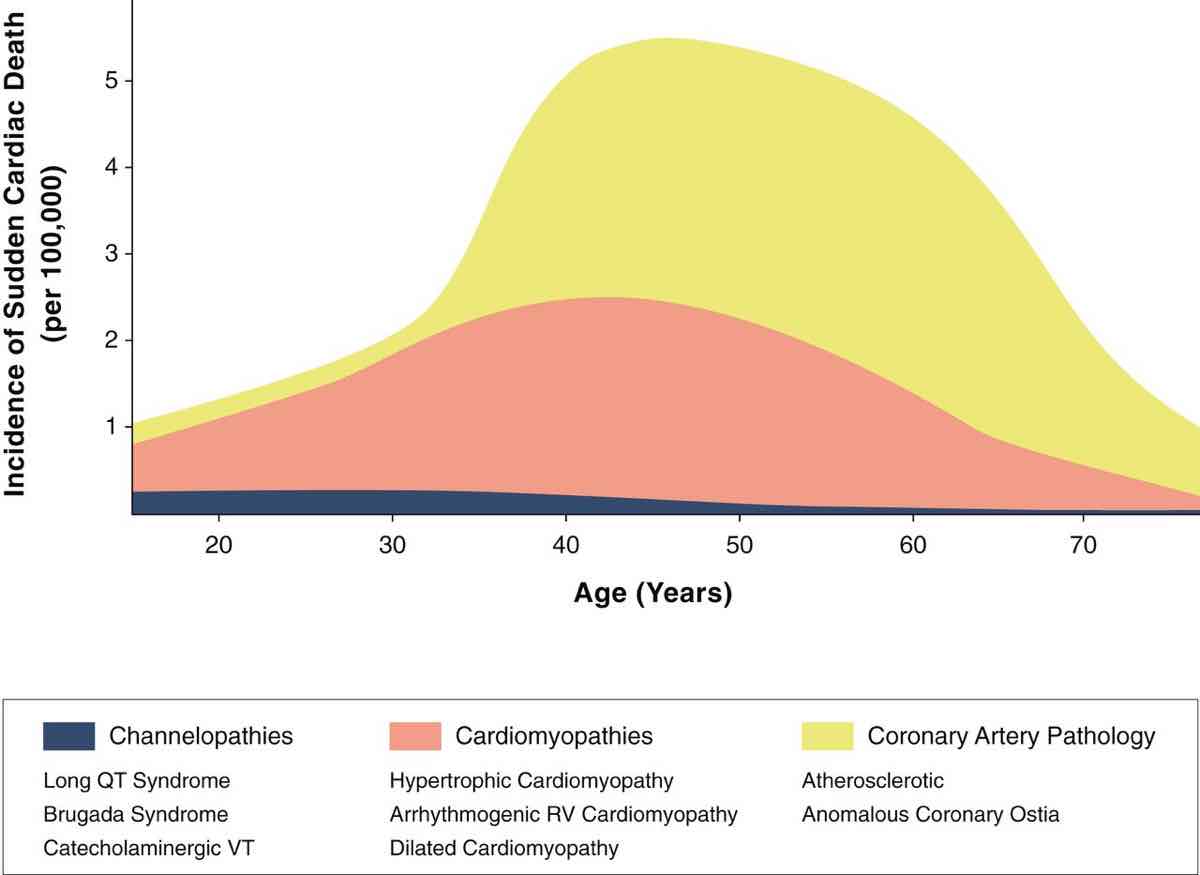
Figure 5. The relationship of channelopathy, cardiomyopathy, and coronary-artery pathology with the incidence of sudden cardiac death. Note that channelopathies and cardiomyopathies both predispose to irregular heartbeats (arrythmias), which can cause the heart to pump ineffectively. Coronary-artery pathology predisposes to “heart attacks” (when the heart does not get enough blood). Image from Cardiac Imaging and Stress Testing Asymptomatic Athletes to Identify Those at Risk of Sudden Cardiac Death. Andre La Gerche, Aaron L. Baggish, Juhani Knuuti, David L. Prior, Sanjay Sharma, Hein Heidbuchel, Paul D. Thompson JACC: Cardiovascular Imaging Sep 2013, 6 (9) 993-1007.
Indeed, as the average age of marathon runners increases and, if more runners with unknown, underlying coronary-artery disease try the marathon distance, we can expect the overall number of marathon-associated sudden cardiac deaths to increase. And this is a good time for my plug for having a defibrillator available at all races, even if races are small. I would also encourage all runners and aid-station workers to get certified in basic life support so they can perform CPR if necessary.
Long-Term Effects of Running on Life Expectancy
Now for the really good news: in a 15-year study comparing runners to non-runners, runners had 45% and 30% lower adjusted risks of cardiovascular and all-cause mortality, respectively, with a three-year overall life-expectancy benefit (Lee, 2014).
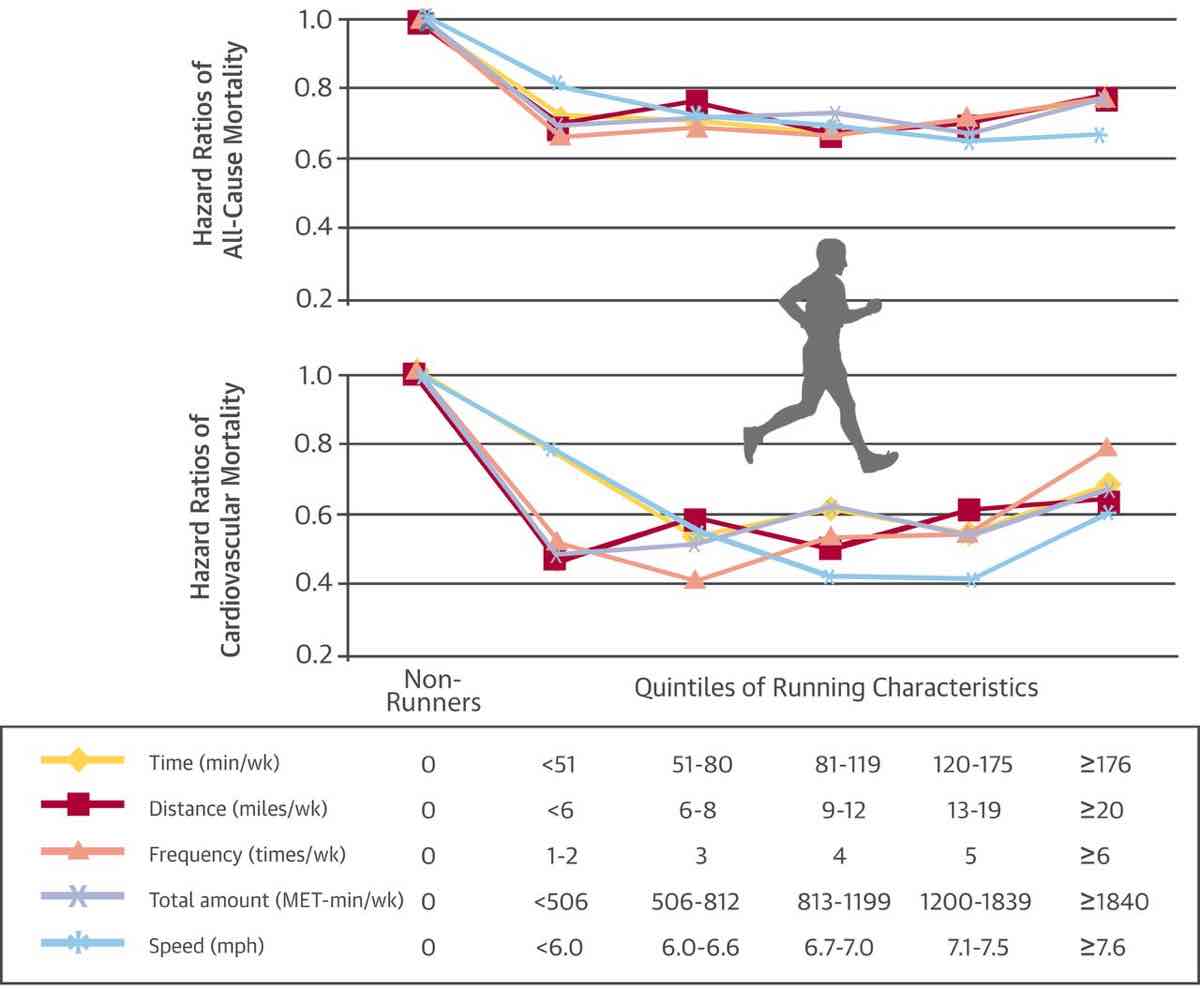
Figure 6. A demonstration that, regardless of speed, distance, or time spent running weekly, runners have lower rates of cardiovascular and all-cause mortality than non-runners. Image from D.C. Lee, R.R. Pate, C.J. Lavie, et al. Leisure-time running reduces all-cause and cardiovascular mortality risk J Am Coll Cardiol, 64 (2014), pp. 472-481.
Another study (Chkravarty, 2008) compared the 21-year survival rate of a runner’s group compared with healthy controls and, even after adjusting for co-variates such as age, the runners had over a 40% survival benefit, which, as shown in Figure 7, continued to widen as the runners aged.
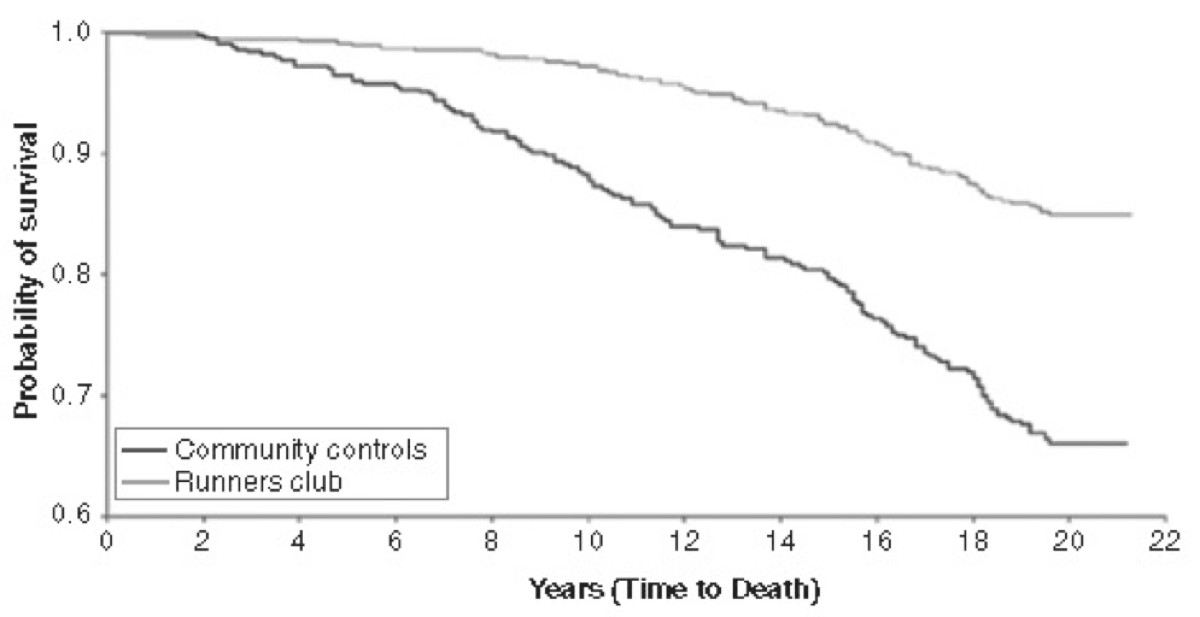
Figure 7. The relationship of runners and non-runners and mortality. Image from Chakravarty EF, Hubert HB, Lingala VB, Fries JF. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168:1638-1646.
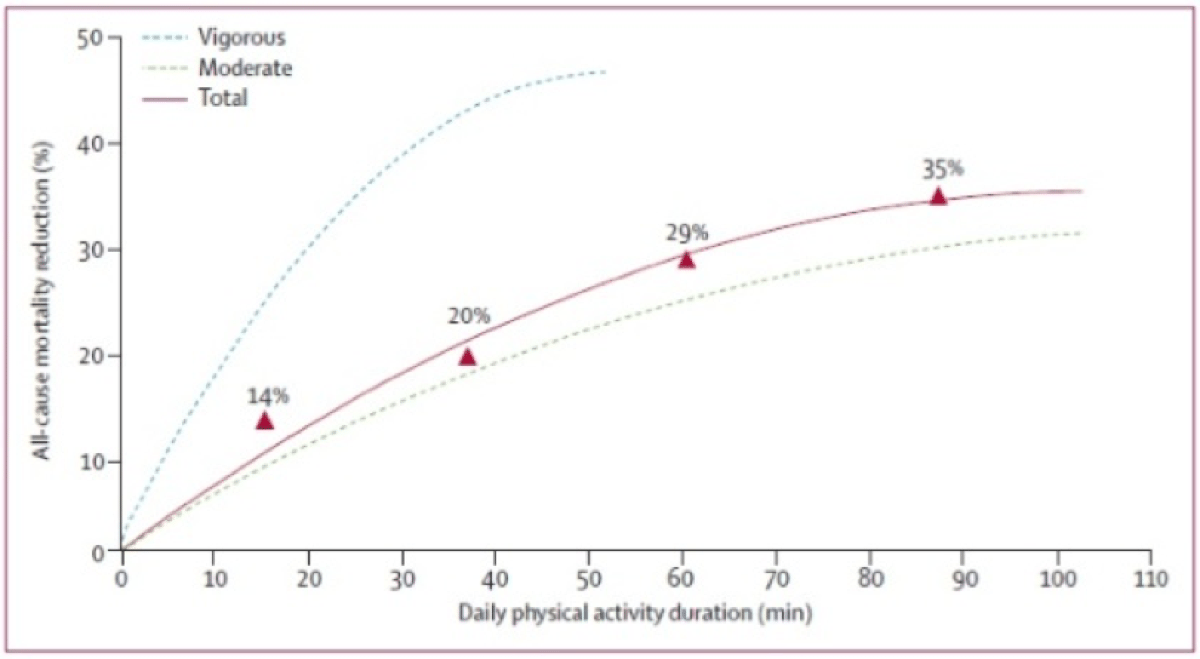
The previously listed benefits do not appear to be unique to running, however, as physical activity in general is associated improved survival (Wen, 2011). This prospective study also showed the more people exercised and the more vigorous it was, the greater their reduction in all-cause mortality (see Figure 8).
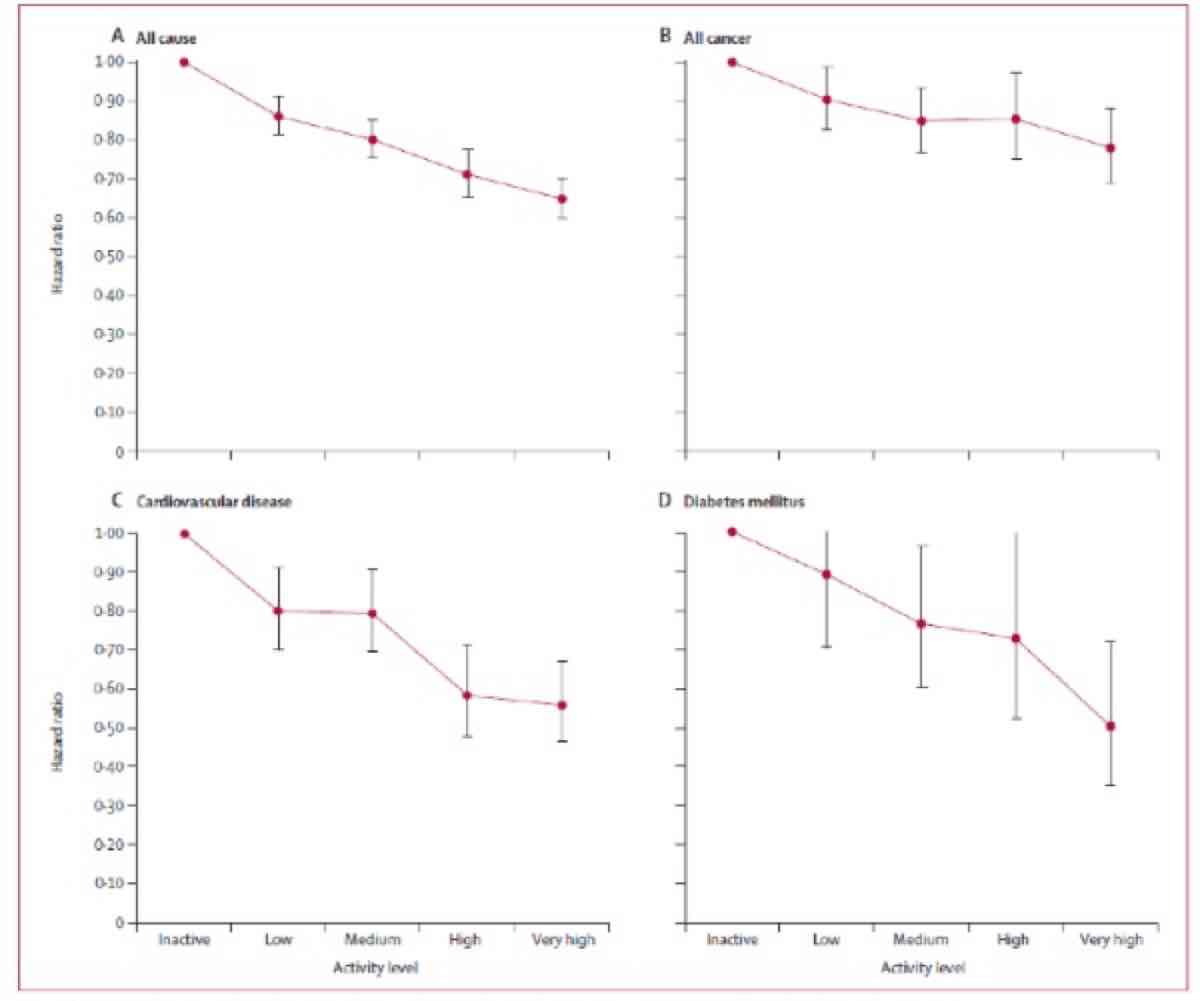
Figures 8 and 9. The relationship between the rate of daily exercise and various health problems. These images show not only a reduction in cardiovascular deaths, but also interestingly in cancer-related deaths and in all causes of death. There appears to be a dose-response relationship where increasing amounts of activity appear to confer a larger survival advantage for the above major causes of death. Both images from Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–53.
Long-Term Changes to the Heart Related to Running
Endurance athletes’ hearts adapt to regular training. The left ventricle enlarges (see Figure 2), allowing it to pump blood more efficiently during exercise. This ‘eccentric hypertrophy’ is important in improving endurance performance and the function of the left ventricle remains normal, even improved, during exercise. The right and left atria also enlarge, which are generally also felt to be physiologic adaptations and, the only major concern presently about these is the enlarged left atrium may be the reason endurance athletes tend to develop atrial fibrillation/flutter. (Read on for more information on this.) Particularly strenuous marathons and ultramarathons have been shown to reduce cardiac function temporarily once the race has finished, but function appears to, without exception, return to baseline within one week, thus strongly suggesting there is no permanent heart damage done (George, 2012).
One thing that has historically concerned physicians about marathon running is the immediate post-race elevation in enzymes that are normally released during a heart attack, including cardiac troponin. However, these laboratory values quickly return to their baseline normal level (within 24 hours) after a marathon and remain elevated for six days after a myocardial infarction (“heart attack”). It is generally felt that the release of these enzymes is inherent to and expected with exercise and potentially a sign of cardiac strain or simply due to increased blood acidity or temperature (George, 2012). The release of these enzymes has not been found to be a sign of permanent heart damage and has not been related to negative health outcomes (George, 2012).
Atrial Fibrillation/Flutter in Endurance Athletes
Unfortunately, there is a growing body of evidence that endurance athletes have a greater prevalence of atrial flutter/fibrillation compared to non-active controls (Mont, 2002; Molina, 2008 Mont, 2009). The most convincing evidence of this was published by Andersen, et al in 2013. They prospectively studied 52,755 long-distance cross-country male skiers, who participated in the Swedish Vasaloppet. As shown in Figure 10, both faster finish time and higher number of races increased the risk of developing an arrhythmia. Specifically, each Vasaloppet completed conferred a 6% increased risk of developing an arrhythmia and faster finishers who had completed five or more Vasaloppets had about a 30% increased risk of arrhythmia. It is important to note that all of the above studies included only men.
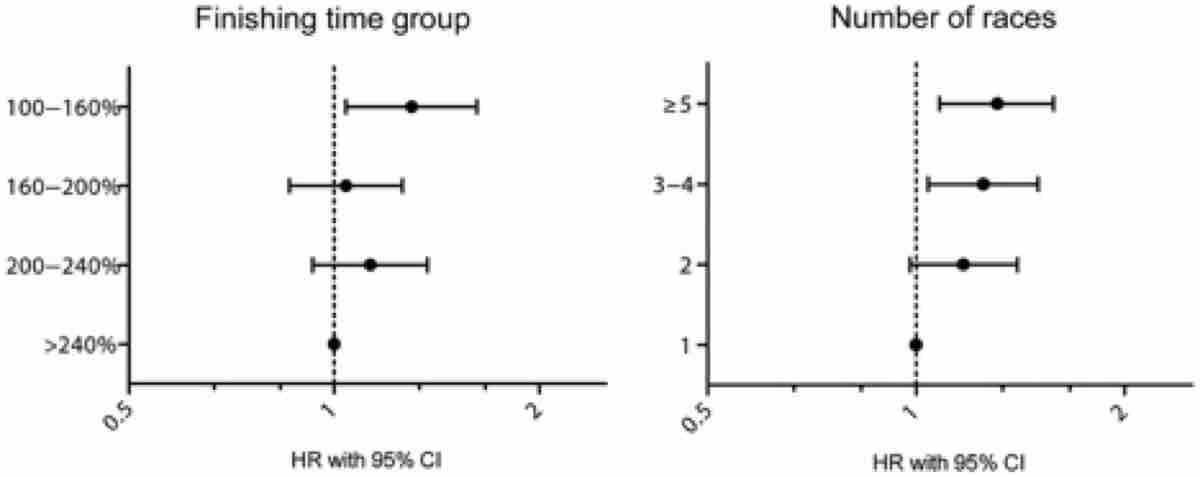
Figure 10. Faster Vasaloppet cross-country ski racers and racers who have competed more than five times both have a significantly increased risk of cardiac arrhythmias. Image from Andersen K, et al. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. European Heart Journal, 2013.
Athlete-Specific Coronary-Artery Disease
Two recent cross-sectional studies from Germany (Merghani, 2017) and Holland (Aengevaeren, 2017) taken together suggest there is a higher prevalence of calcific-type coronary-artery plaques among athletes, especially those with the most exercise exposure. This plaque type has been found to be more stable (less likely to cause myocardial infarction) and there are currently no data to suggest that these specific plaques in an athletic population are associated with negative health outcomes. In an editorial (Baggish & Levine, 2017), it is suggested this plaque morphology may be yet another “benign” adaptation to exercise. More data are needed to draw conclusions, but Michael Joyner, MD, an anesthesiologist sports researcher at the Mayo Clinic states “stable plaque plus larger coronary arteries that dilate more in high-volume exercisers should be highly protective against coronary events” (Huston, 2017).
Which Runners Should be Screened for Cardiovascular Risk and How?
The American College of Cardiology currently recommends the following for adults prior to starting a new exercise program (Perritz, 2017):
“From a public health perspective, the sensitivity of screening entire populations is too low to be cost-effective. Similarly, it would not be feasible to require testing prior to participation in large events, such as marathons in major cities. Instead… exercise testing would be appropriate to consider in the following circumstances: 1) in people >35 years with significant risk factors for coronary disease (diabetes, elevated cholesterol, hypertension, obesity) prior to initiating a new exercise regimen; 2) to attempt to reproduce symptoms (such as chest pain, irregular heart beats, etc.) associated with exercise in any patient; or 3) to test exercise capacity in anyone who has noted a change in performance without other clear causes.”
Screening electrocardiograms (EKGs) are often expected to be part of the pre-participation physical in Europe, however. This is based upon recommendations by both the European Society for Cardiology and International Olympic Committee. This is largely because of the findings of an Italian study (Corrado, 2007) that was able to show a reduction in cardiac death after the initiation of EKG screening. Screening EKGs are not recommended by the American Heart Association or the American College of Cardiology based on a similar American study (Steinvill, 2011) which found that mandatory EKG pre-participation screening did not reduce the rate of cardiac death. It should be mentioned that the Italian study was prospective and could determine cause, whereas the American study was retrospective and could only find an association.
Conclusion
In conclusion, there is overwhelming evidence that regular endurance exercise is associated with reduced risk of cardiovascular and all-cause mortality. If you do not have an underlying heart condition or disease, your risk of sudden cardiac death during a race is essentially zero. There should be no generalized recommendation for adults or children to reduce exposure to running or exercise. So go ahead, keep running (!), and on a rest day, consider getting certified in basic life support.
Call for Comments (from Meghan)
- Your heart and your running, what can you tell us about it? What have you learned from your physician about the condition of your heart over the years? And has your heart changed over your lifetime as a runner?
- Have you seen a cardiac event at an ultramarathon? Can you share what you observed?
References
Andersen K, et al.. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. European Heart Journal, 2013.
Chakravarty EF, Hubert HB, Lingala VB, Fries JF. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168:1638-1646.
Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006 Oct 4; 296(13):1593-601.
Dewall, Natahn. Running in the Sahar https://www.nytimes.com/2017/06/02/well/move/running-in-the-sahara.html
George K, Whyte GP, Green DJ, et al The endurance athletes heart: acute stress and chronic adaptation Br J Sports Med 2012;46:i29-i36.
Hicks, M. Personal communication. 2018.
Huston, L. Coronary artery calcium rises with intense exercise. Cardio Brief. 7/13/2017. https://www.cardiobrief.org/2017/07/13/coronary-artery-calcium-rises-with-intense-exercise/.
Kim et al. Cardiac Arrest During Long Distance Running Races. N Engl J Med 2012; 366:130-140.
Lee DC, et al. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol, 64 (2014), pp. 472-481
Marathon des Sables Training Blog. https://mds2008.blogspot.com/2007/04/death-on-marathon-des-sables.html.
Molina L, Mont L, Marrugat J, et al. Long-term endurance sport practice increases the incidence of lone atrial fibrillation in men: a follow-up study. Europace 2008;10:618–23.
Mont L, Sambola A, Brugada J, et al. Long-lasting sport practice and lone atrial fibrillation. Eur Heart J 2002;23:477–82.