Working from home or a lost job altogether, extended school cancellations, large-event cancellations months into the future, no non-essential travel allowed, significant illness among our loved ones, and so much more: the COVID-19 pandemic has affected nearly every part of everyone’s life.
Not only have the lives of us runners been upended, but so has our running. At this point, races have basically been canceled or postponed globally through the end of June, with even the 2020 Summer Olympics which were scheduled for August off the calendar for now. Run training and social gatherings have been suspended. And in most places around the world there are government restrictions and recommendations on how we can exercise.
What we know about COVID-19 and how each of us should modify our behavior to decrease the risk of its spread changes on the daily. We all still need to know the answers to these crucial questions:
- What is COVID-19 and how does it ‘work?’
- What is our personal risk of illness from it?
- What is our responsibility to the wider community in helping to prevent others from getting sick?
We continue to update this article with answers to these questions using the scientific community’s current knowledge.
[Editor’s Note: This article was originally published on Saturday, March 14, and last updated on Wednesday, April 15.]
What is COVID-19?
COVID-19 comes from a large family of viruses known as coronaviruses. They get their name ‘corona’ because of the crown-like spikes on their surface. Coronaviruses cause a range of respiratory illnesses from the common cold, to much more severe diseases such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) (5). Given that coronaviruses cause serious respiratory diseases, organizations like the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) monitor populations for unusual disease clusters. With COVID-19, an aggregate of viral pneumonia cases was linked to an animal market in Wuhan, China and determined to be a novel coronavirus (one not circulating in humans prior to this outbreak). What started in one market in China has quickly spread globally. This is called a spillover event and happens when the virus moves from its animal host into the human population. According to Johns Hopkins University’s COVID-19 live tracker, as of Wednesday, April 15, over 2 million cases are confirmed in 185 countries and regions.
Why Is COVID-19 Giving Us the ‘Run Around?’
COVID-19 is a serious illness. To help us understand this, we look at available data on how contagious it is, how easy it is to transmit, and the severity of its symptoms. We also compare these data to that of the seasonal flu, another virus we all know well.
COVID-19 Is Highly Contagious.
Every infectious disease has something called the R0, pronounced ‘R naught,’ which is the mathematical term indicating how contagious it is. Since the infection literally reproduces itself as it spreads to new people, sometimes this is referred to as its reproduction number. The R0 tells us the average number of people who are likely to catch a disease from one infected individual, and it varies among specific populations based on interventions taken against it. Generally speaking, if R0 falls below 1, the disease will naturally die out in the population (7).
The current R0 of COVID-19 outside of China is between 2.2 and 2.7, meaning that every infected person will likely infect 2 to 3 additional people. However, without interventions (social-distancing measures and more), the R0 is estimated to be closer to 5.7 which might explain its rapid initial spread (14). For comparison, the average R0 of the seasonal flu is 1.3 (6).
Importantly, R0 is not a set-in-stone number, and it changes over the course of a disease’s spread. For example, the R0 for COVID-19 in China is approaching 1. They’ve managed this via enormous interventions including enforced social distancing and developing testing that allowed for more than a million people to be tested each week (6). One of the best examples of a rapid and effective response is Singapore which now has a COVID-19 R0 of 0.3 largely due to their radical transparency, rapid testing, strict social distancing, and effective quarantines (6, 8).
COVID-19 Is Easy to Transmit.
One of the reasons COVID-19 is spreading so rapidly is at least partially due to the fact that you (yes, you, right now) might be carrying and actively shedding (releasing active viral particles/droplets) and not even know it (1). Most people who are infected with COVID-19 will develop symptoms 5 to 12 days after becoming infected. However, peak virus shedding happens early in COVID-19 (2 to 5 days post-infection). This means you could be actively contagious for up to 10 days before showing symptoms (1, 9). In contrast, you will show symptoms of the seasonal flu 1 to 4 days post-infection and become contagious 24 hours before your symptoms appear.
COVID-19 Causes Serious Symptoms.
There is still much that is unknown when it comes to COVID-19, some of which will not become clear until we’ve come out the other side (due to under testing, asymptomatic-but-infected individuals, and more), and this includes the virus’s ultimate mortality rate. What we know so far is that COVID-19 has very serious symptoms. The current rate of hospitalization for COVID-19 patients in China and Italy is 10 to 15% (13). There are university reports that this could be higher in the 65-and-older population, with 20 to 24% of this demographic’s COVID-19-positive patients requiring hospitalization. Again, these numbers will become more clear when this is all over due to limitations in testing. For comparison, the CDC estimates that in an average year, 1.0 to 1.8% of seasonal-flu-positive patients require hospitalization. And the hospitalization rate for the ongoing 2019-2020 flu season is estimated at 1.0 to 1.3% (12).
How Is COVID-19 Transmitted?
The coronaviruses, including COVID-19, are spread from person to person via respiratory-droplet transmission. Every time an infected individual coughs, sneezes, yells, or even breathes, they release infected droplets into the environment up to about 6 feet away–and possibly even further. This distance of 6 feet comes from standard medical precautions for any disease spread via droplets, including the common cold and other coronaviruses. We are learning that droplets may travel further than 6 feet in some situations, and so we should consider this to be truly a minimum precaution. Additionally, COVID-19 viral particles can live on some surfaces for up to 3 days (11), so even if you were not in the direct line of fire from a cough or sneeze, you can still pick up infected droplets from other surfaces they have landed upon and transport them to your face (eyes, nose, or mouth) via your hands. We should also keep in mind that a lot of virology still needs to be done (and is actively being done) to determine how virulent COVID-19 is. Virulence refers to how many viral particles are needed to get someone sick. For example, measles is highly virulent and requires a very low number of particles to infect someone, whereas the common cold or flu requires more viral particles to sufficiently infect an individual.
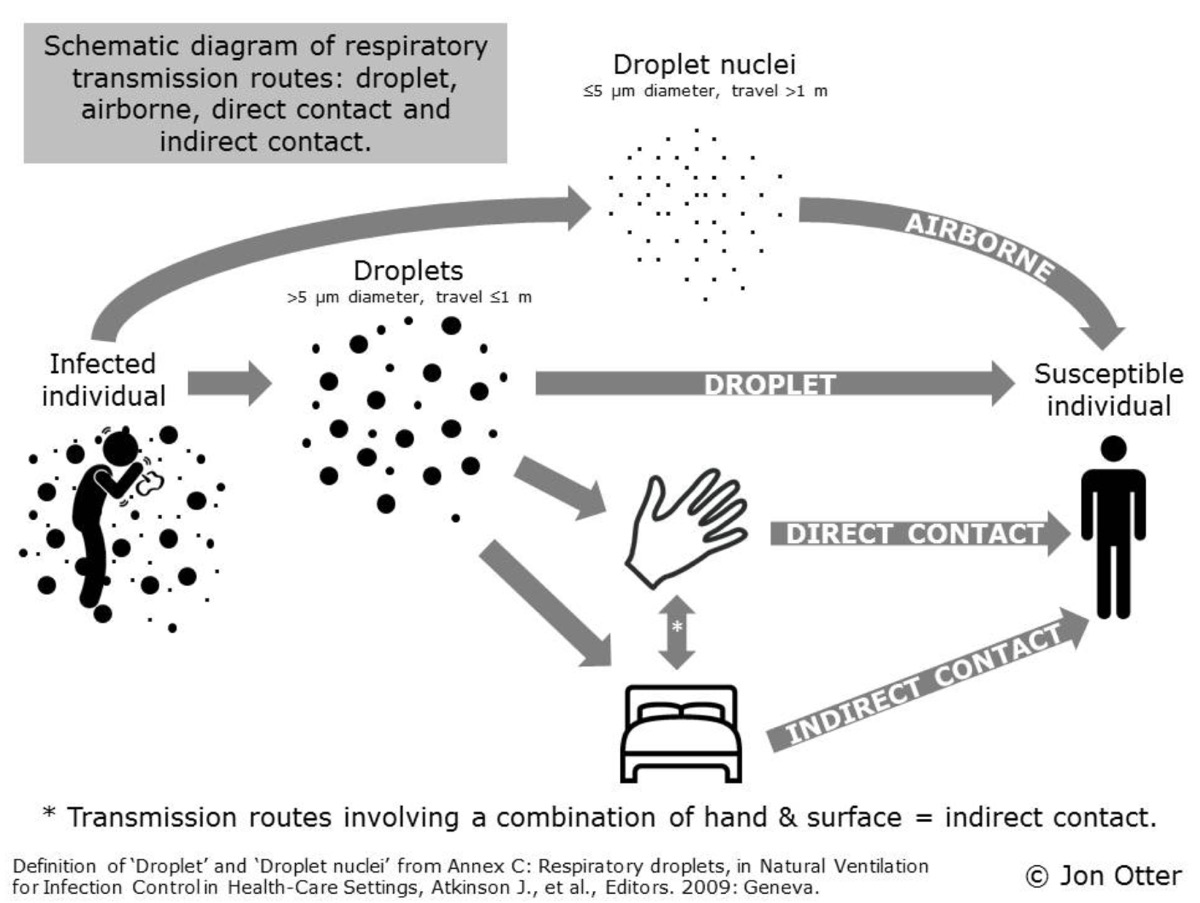
How COVID-19 is transmitted. Image: Otter, Jon. “Surface Contamination and Respiratory Viruses with Pandemic Potential (SARS, MERS and Influenza): an Underestimated Reservoir?” Reflections on Infection Prevention and Control, 16 Dec. 2015, reflectionsipc.com/2015/12/16/surface-contamination-and-respiratory-viruses-with-pandemic-potential-sars-mers-and-influenza-an-underestimated-reservoir/.
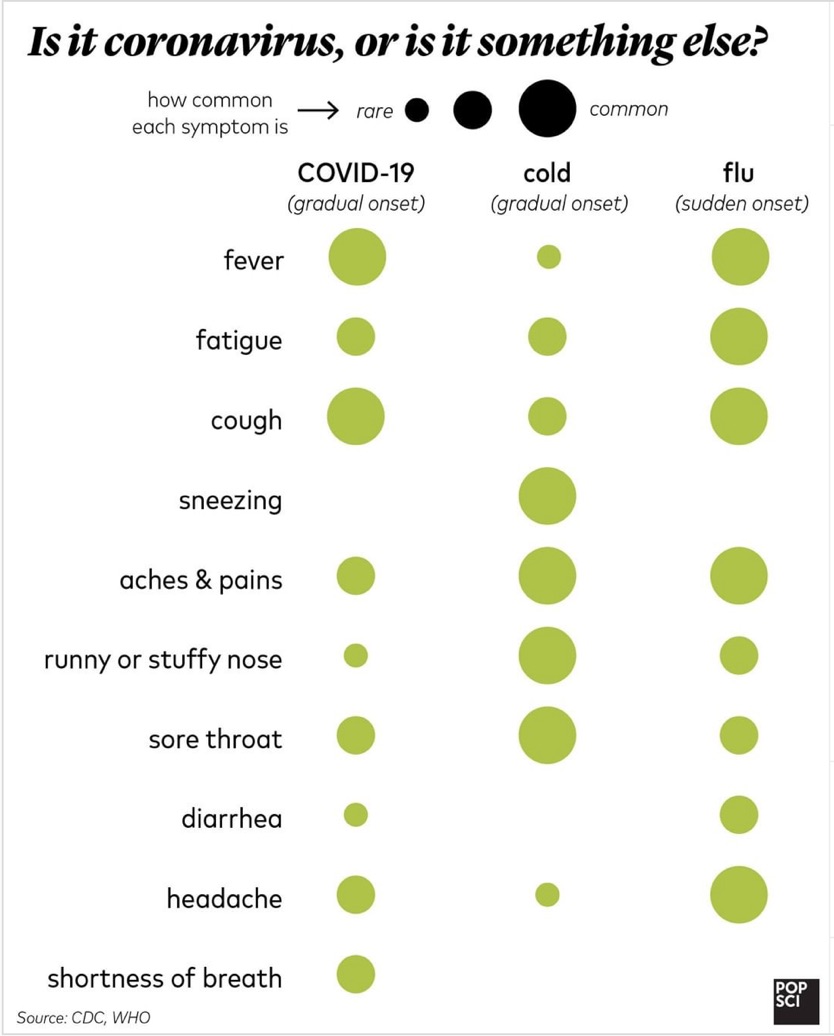
A comparison of COVID-19, common-cold, and seasonal-flu symptoms. Image: Baggaley, K. (2020, March 11). COVID-19 symptoms typically appear 5 days after infection. Retrieved from https://www.popsci.com/story/health/coronavirus-incubation-period-time-symptoms/
Why Should Each of Us Take Action in the COVID-19 Pandemic?
For as much panic as I’ve witnessed over the past couple months, I’ve also witnessed an equal amount of ambivalence. How much danger is each of us actually in? What it looks like right now is that if you are under the age of 50 and do not have other risk factors such as a history of smoking, a compromised immune system, cardiovascular disease, or any other chronic illness, you are much less likely to require hospitalization or intensive care (2, 6). What this means is that if you become infected, you will likely only experience mild symptoms (as in about 80% of the cases in China) or even be asymptomatic–the latter a problem all its own as we’ve explained. Symptoms can range from being down with a bad cold to “getting hit by a truck,” as was described to me by a friend. The big difference between riding this out at home versus requiring medical care has been coming down to people experiencing shortness of breath and low oxygen saturation (how well oxygenated your blood is).
There are also a lot of people reading this who are older than 50 or who have health conditions. And we all know and spend time with people who are and do. These are the people who are most vulnerable to becoming severely ill as a result of COVID-19. Thus, how each of us individually and how our whole community responds matters. I urge you to not panic, but I also urge you to take pause and reflect on how you can help the vulnerable of all our communities. Piggybacking off our climate-change conversations, I’ve been asking myself, How can I limit my COVID-19 ‘footprint?’
Because me paraphrasing will not adequately do it justice, I’ll quote Zeynep Tufekci (3) in Scientific American, “Preparing for the almost inevitable global spread of this virus… is one of the most pro-social, altruistic things you can do. We should prepare, not because we may feel personally at risk but so that we can help lessen the risk for everyone. We should prepare not because we are facing a doomsday scenario out of our control, but because we can alter every aspect of this risk we face as a society. That’s right, you should prepare because your neighbors need you to prepare–especially your elderly neighbors, your neighbors who work at hospitals, your neighbors with chronic illnesses, and your neighbors who may not have the means or the time to prepare because of lack of resources or time.”
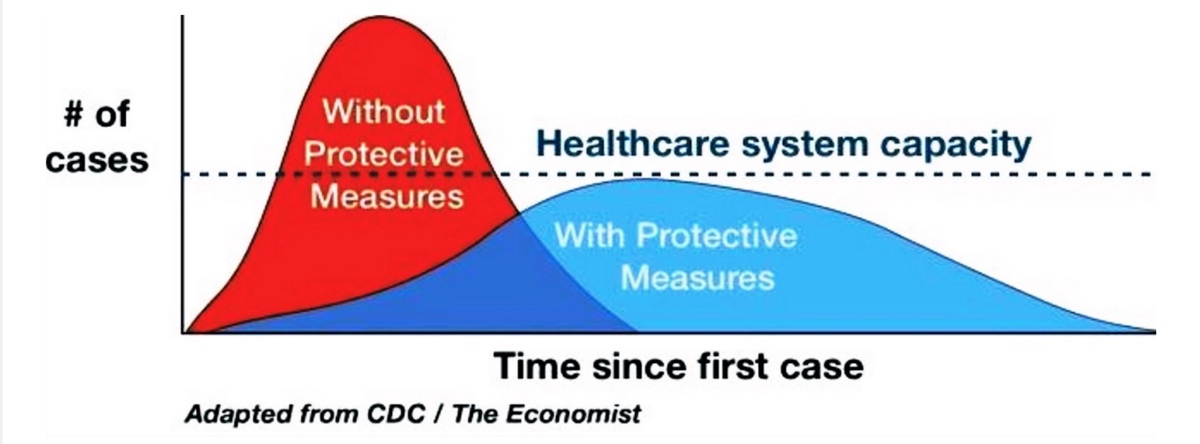
What ‘flattening the curve’ means. Image: FlattenTheCurve.com. (2020, March 9). FlattenTheCurve: COVID19 Update & Guidance to Limit Spread. Retrieved from https://www.flattenthecurve.com/
What we need to do is to interfere with the natural flow of the COVID-19 outbreak by slowing its spread (4). This is what the scientific community calls ‘flattening the curve’ or reducing the number of active cases at any given time.
This is important because it not only decreases the overall number of people who become ill, but it can also prevent our health-care systems from being overwhelmed. Simple math tells us that no community’s health-care system is large enough to support COVID-19’s natural spread. Left to its own progression, it will create many more seriously sick people than can be properly cared for. Flattening the curve puts fewer people into the health-care system at one time, and helps allow everyone to get care that matches their illness’s severity. This will avoid unnecessary deaths.
I feel fortunate to live in California, a U.S. state that has acted aggressively and quickly to mandate social-distancing and sheltering-in-place orders. As of April 15 and despite the state having high population density in many places, the orders have been seemingly effective in flattening the curve in the San Francisco Bay Area counties.
Social Distancing Is Everyone’s Responsibility.
There is hope! We have tools that each of us can employ to help prevent COVID-19’s spread. From both past pandemics and watching countries react well and poorly to the COVID-19 pandemic, we know that social distancing is perhaps the most effective tool available to us.
Simply put, social distancing is intentionally staying away from other people in order to avoid catching and spreading a virus. This means maintaining enough distance between yourself and other people (a minimum of 6 feet) as well as limiting large, close gatherings of people. Examples of the latter include concerts, school, large offices (hello working from home!), conferences, meetings, busy restaurants and stores, and, yes, even running events. While it is thought that there is likely more risk in being inside with large groups than outside, social-distancing practices include limiting large numbers of people anywhere.
As of April 7, all but 5 U.S. states have issued shelter-in-place or safer-at-home instructions, which accounts for 95% of the U.S. population (15). The current instructions generally state that residents can leave for essential work, errands (grocery shopping and medical appointments), and exercise. The mandates are different in every state and city but have widely tried to enforce social distancing without going into more aggressive lockdowns like in many Asian and several European countries. Some states have gone further to shut down public land, closing trailheads and wild spaces, to limit both congregating and the need for remote emergency rescues stressing potentially overtaxed healthcare systems.
Large-group events, including races, are currently not permitted. On Sunday, March 15, the CDC recommended that for 8 weeks, large groups be limited to under 50 people. On the same day, Ultra-Endurance Sports Science & Medicine, a non-profit group of sports researchers and physicians, recommended that endurance sports limit large groups to under 50 people through June 15 or for 3 months, with a reassessment for extending the time period on May 15. They further recommend that if an event with under 50 people is still held during this time, participant use of public transport to the event is discouraged. On Monday, March 16, the U.S. White House recommended gathering no more than 10 people together and to practice strict social distancing in doing so.
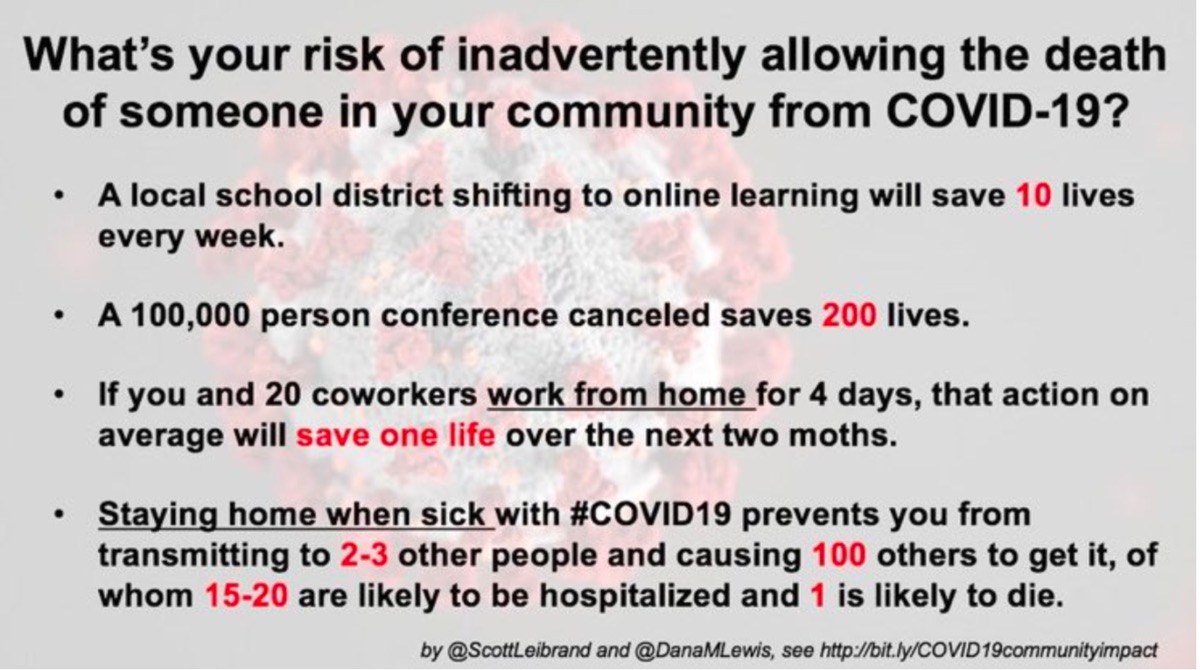
How your actions during the COVID-19 pandemic can affect your community. Image: FlattenTheCurve.com. (2020, March 9). FlattenTheCurve: COVID19 Update & Guidance to Limit Spread. Retrieved from https://www.flattenthecurve.com/
But We’re Trail Runners and Ultrarunners!
There’s been a lot of talk about canceled and postponed races and events. There have also been plenty of jokes to the effect of, “I got into running for the social distancing!” or “Trail runners won’t get COVID-19 because no one else is out in the woods at 6 a.m.” While there is some validity to both those statements, in jest or not, do you as a trail runner need to be worried? Are these race directors crazy? Should I stop putting my hand directly into the food bowls at the aid station?
Immunologist and ultrarunner Eric Lee confirms that trail running is generally safe–we’re outside and usually away from large crowds (check, check). But he also confirms that ultrarunners aren’t exactly known for their excellent hygiene. What he means is that in a trail/ultramarathon race setting, hygiene (even outside of a pandemic) is less than ideal. Even though we are not running in the same density of people as you would in a metropolitan road race, we are given ample opportunity to unknowingly spread disease. Explains Lee, “During races, we share common food dishes, fill our water bottles from the same containers, have direct contact with many people, and share plenty of hugs and high fives.”
Also, is there inherent risk to running or racing long distances during a pandemic? While it’s true that hard training and racing causes short-term immune-system suppression, that depression is short lived and your immune system bounces back quickly. What that means, says Lee, is that there is a short window (post-exhaustive training/racing) where you are theoretically more susceptible to infection, but your immune system is robust and dynamic, and will quickly right the ship.
Yes, runners, you may keep running so long as you keep your social distance by running alone or with only one member of your household! (There are a few places in the world where running in public is currently not permitted due to quarantine rules. Please follow your local regulations.) However, the canceling and postponement of races are in the best interest of our broader community. Social distancing and limiting large numbers of people gathering, be it in shuttles to the race start or at the finish-line after party, have still been shown to be one of the most effective ways of slowing the spread of viruses like COVID-19. Plus there is the now-well-known risk of COVID-19 infection via travel (which we will talk about shortly), which racing often requires.
What Else Can We Do to Flatten the COVID-19 Infection Curve?
Here are more actions we can all take to help reduce the spread of COVID-19.
Choose Running Routes Wisely.
Please follow your local, state, and federal guidelines when it comes to getting outside responsibly. These guidelines will continue to change daily, and what might have been okay a week ago might not be okay today or tomorrow. If your trails are still open, I encourage you to go during off-peak hours, run alone, and avoid narrow trails where it’s hard to give yourself and others space. This is additionally a time to pick safe routes and to be aware of remoteness, terrain conditions, and more. They’re called accidents for a reason.
Wear Masks and Face-Coverings Responsibly.
On April 4, the CDC recommended using masks or face-coverings in public settings where social distancing is difficult to maintain. So how and when should we use masks?
First and foremost, reserve sterile (not yet opened) N95 and surgical masks for people with high exposure rates (think healthcare workers, first responders, and other essential workers including the folks working at your local grocery store). It turns out that cloth masks are fairly effective at limiting the emission of viral particles by up to 30% if you were to sneeze or cough while wearing one (16, 17). It’s not perfect, but it is a big reduction, particularly if you remember we are wearing masks to protect those around us while in close spaces.
Now, do you need to wear a mask while exercising? If you are running alone and practicing social distancing, it’s likely unnecessary. Plus, once a cloth mask gets wet (as you breathe through it, and this happens fairly quickly), it is no longer an effective barrier for respiratory particles. Another point for social distancing! However, having a covering like a buff or bandana that you wear around your neck, keep mostly dry there, and pull up temporarily as you pass other people may be the most practical, effective, and polite way we runners can currently use masks.
In general, getting into the habit of wearing a mask in public spaces is a good idea. Remember that you still need to wash your hands and practice good hygiene. This includes putting the mask on before entering a public space and refraining from adjusting the mask once it’s on. Once you are back home or in a safe space, remove your mask and sanitize your hands again.
Join the Hand-Washing Revolution.
Let’s continue to practice good hygiene. As a reminder, the CDC recommends that you wash your hands before, during, and after preparing food; before eating; before and after caring for someone who is sick; before and after treating a wound; after using the toilet; after changing diapers; after blowing your nose, coughing, or sneezing; after touching an animal, animal feed, or animal waste; and after touching garbage. Additionally, wash your hands with soap and warm water for more than 20 seconds, or the time it takes to sing “Happy Birthday” twice, or if you are feeling spicy the choruses of “Truth Hurts” by Lizzo or “Raspberry Beret” by Prince. Use hand sanitizer when you’re unable to wash your hands regularly.
Stop Touching Your Face.
The most common way a virus enters your body is through your eyes, nose, and mouth, so stop touching things that may have respiratory droplets on them and then touching your mustache, or picking your nose, or whatever else you are doing around there. If I’ve learned anything in the past two weeks, it’s that I touch my face, a lot. I’m working on this one.
Limit Touching Other People and Surfaces.
Stop shaking hands. My new personal favorite is the foot-five, but I’d take a princess wave, a bow, or a curtsey. Work on your elbow dexterity for pushing open doors, utilize those sleeves, and keep your fingertips away from light switches.
Clean Frequently Touched Surfaces.
Focus on surfaces both at work and home. Disinfect screens (like your phone!), counters, door knobs and handles, and light switches. This should also include cleaning yourself once you arrive home.
Stay Home If You Are Sick.
If you are sick, stay home. If you are sick enough to seek medical care, follow local protocol during these pandemic conditions. This may mean calling your primary-care provider or perhaps a hotline set up for your region. Limit your risk of infecting others by responsibly isolating yourself while contagious. And this should go without saying, but if you have come into contact with someone who has tested positive for COVID-19, self-quarantine for 14 days while monitoring for symptoms.
Don’t Travel Unless It’s Essential.
Travel is a significant part of how COVID-19 has so quickly spread worldwide. Given current shelter-in-place mandates, almost no travel is happening right now. As we begin to come out of peak infection rates in the coming weeks, this recommendation will likely remain important.
Be Kind, Calm, and Pliable.
Make plans to help out older family and community members, and anyone who is vulnerable. If your race has been canceled, consider donating your race-entry fee to the race director to help ease the financial burden of their last-minute cancelation. Do what you can to support the people in your community whose livelihoods are most heavily impacted by this process.
Remember to be kind to yourself and others in these tumultuous times. Stress is an immunosuppressant (10), which is why I am here yelling, “I’m trying so hard to relax right now!”
This situation is rapidly changing. As scientists learn more, recommendations may change and perhaps become more restrictive. Listen to the experts.
It’s About More Than You.
This is bigger than you; it’s bigger than any of us. We need to normalize this being ‘everybody’s problem.’ This means following local, state, national, and international guidance. Many of us runners are at low risk of getting very sick from COVID-19, but we are surrounded by people who are not. Our actions affect everyone.
A Message from Italian Trail Runner Martina Valmassoi
On March 14, Trail runner Martina Valmassoi shared what life is now like in her hometown in the Veneto region of Italy due to the COVID-19 pandemic, the country’s major loss of life and health, and government quarantines to try and slow its spread:
“More or less, here’s what has happened. This time last weekend, I was traveling to a ski-mountaineering race in Trento two hours away. At that time, we were talking about the virus and understanding that they have to prevent the spread, but none of us really understood what was going on for real. Two days later, I was ‘locked’ inside my house.
“Last Sunday, something changed. They stopped calling COVID-19 a stronger flu. We finally realized that lots of people and not just elderly people were dying for real. We [finally understood] that the request of isolation was necessary to protect the weakest. Once you understand that with the contact of other people you might infect your grandparents or parents, you definitely change your behavior. The biggest problem here besides the virus itself is the capacity of the hospitals and the number of [ventilators.] It’s super scary.
“Imagine this scenario. You go out you meet someone you don’t know is infected. You go home. You infect your parents. They visit grandma to bring her food. All now are infected. At some point, we all need to go to intensive therapy [at the hospital] because we couldn’t breathe without. There are not enough hospital places, so they give priority to the one with more chances to live. You get the spot. Your parents and grandma are dying because you didn’t stay home.
“Yes, we are staying inside as much as possible. I live in a mountain town in [the region of] Veneto, with not much people so for us it’s not as hard as it could be in the city. Also, we don’t have any contagious problem yet [in my town], but this can change at any minute. Cafes are closed, restaurants too. Supermarkets and pharmacies are still open but you have to respect the safety distance [between each person]. We can’t drive outside our village, so we must get groceries in our village. Most of the factories have closed, but a few people are still working. You can go out to walk the dog and ‘for health,’ but always close to your house and not for long. Skiing, climbing, and running are not accepted because they might be dangerous and they don’t want to rescue people. Right now, we should be isolated until the third of April, but we don’t know if this will change and we are actually fearing it. Not everyone is being respectful and responsible. Right now the most affected region is the Lombardia with Bergamo with the most cases. My region has a bronze medal [because we have fewer infections] for now. We will see.”
A Message from American Ultrarunner and Emergency-Room Nurse Scott Brockmeier
On March 19, American ultrarunner and emergency-room nurse Scott Brockmeier shares his thoughts on how the hospital at which he works in Moab, Utah has prepared for COVID-19 and what could happen if the virus moved unchecked through his rural community:
“Here’s my front-line perspective as a med-surg nurse at Moab Regional Hospital (MRH), a small, rural-access hospital in southeast Utah. My 10-plus-year nursing experience has been almost exclusively working in intensive care, but I took a position here in Moab after several years of travel nursing. It’s been a big change for me but I have to give a huge shout out to the administration at MRH. They have been proactive, excellent at communicating with and taking input from the staff, they were one of the first in the state I believe that had a triage tent set up outside the emergency department, and just in general very supportive. There are constant policy changes and it can be confusing and unnerving when it doesn’t seem like anyone knows what is going on but this is an evolving novel virus that does not act like many other viruses and this same kind of changing messaging is happening at the national level. I have 100% faith that the administration is doing the very best that they can and taking care of the staff in the very best way that they can. So, a huge shout out to everyone at the hospital for all their hard work.
“So far at MRH there has not been a confirmed case of COVID-19 and while we’ve been more or less busy it has mostly been the usual patient population though we have had a number of patients that we put on isolation while they were tested. All have been cleared. But I believe that this is the calm before the storm. I do hold out hope that with the county being shut down yesterday (bars and restaurants closed except curbside, hotels not able to hire rooms for non-essential reasons, and all public lands closed to non-resident camping) and our geographical isolation will let us escape our hospital being totally overwhelmed. But that is not a strong hope. I’ve been thinking about what it will be like when people start getting sick and requiring hospital care. We only have 17 med-surg beds, 3 ventilators, and 2 to 3 biPAP machines, so it won’t take much to fill us up. Many patients get shipped out who are gravely injured or critically ill because we are not set up to do many things that larger facilities can do. If this region is hit hard and all of the intensive-care beds fill, then we will not be able to ship them out and will just have to do the best we can with what we have. One of the things I dread most about this coming storm is having to ease the dying of those who need a ventilator but cannot get one. I’ve seen people die by slow suffocation from end-stage chronic obstructive pulmonary disease (COPD) and it is awful. I hope that can be avoided.
“As the author says, this virus is extremely contagious due to the fact that it can hang in the air for hours and on surfaces for days. Having the entire unit full of these patients will make keeping things and ourselves perfectly clean nearly impossible. Add to that the rationing of personal-protective equipment which can only increase the chance of cross-contamination of patients and staff because they need to be reused and are difficult if not impossible to clean. CDC and WHO recommend airborne isolation and gowns for any procedures done on COVID-19-positive patients that produce aerosols. I don’t know if nebulized breathing treatments will help patients with this disease but if they do then not very many patients will be able to follow guidelines because part of airborne isolation is to have the patient in a negative-pressure room and we only have two at MRH. Gowns could also be a problem as they are one-time use. I do remember my manager saying something about reusable/washable gowns, but I’m not sure how that would work. We are also rationing N-95 masks which are meant to be disposable though recommendations say that they can be worn for multiple hours safely. It’s possible that cross-contamination may end up not being something that we worry about if everyone has the same bug. Other factors that will make keeping the unit clean difficult is that we will be full, we will be short staffed with many out sick, and some of these patients may be critically ill without a critical-care bed to send them to. All this makes me think that I need to resign myself to being exposed and we are going to have to figure out how to deal with staff shortages perhaps by having people who are infected but not too ill working. I’ve seen talk of other hospitals taking certain floors and staffing them with dedicated COVID staff and only COVID patients. At MRH we only have one floor/unit, so will it become a locked-down quarantine ward? I don’t know. I don’t know how any of this is going to go down and that may be the most stressful thing right now… the uncertainty.”
Stories of Trail Runners Who Are COVID-19 Positive
On April 15, I spoke with two trail runners who tested positive for and have recovered from COVID-19.
Jon Frias is a 28-year-old runner from New Jersey who became ill in mid-March. This was before the U.S. East Coast shuttered at home, and Jon’s family had a small get-together for his father’s 70th birthday. Within a week, several family members–all young people–were sick. Jon’s symptoms came on suddenly. He can clearly remember being at a grocery store and thinking, I need to get home. I feel really terrible. He had a fever of 101 degrees Fahrenheit.
Jon quickly isolated himself from his parents, with whom he lives. Next, he contacted his primary-care provider, which had COVID-19 tests available. For 4 days, Jon says his fever ranged from 101 to 104 degrees, that he could barely get off the couch, and that he’d never been as sick before. He gradually improved and received his positive test result on day 10.
Being a young, hungry runner who was feeling better, he attempted a short run–he lives in a rural area so could be totally distanced in doing so–but his primary-care provider and coach reined him in. Jon agreed to not run for the rest of the month, which would be 3 weeks off. Jon returned to running on April 1, with short runs focusing on easy movement. Returning to running slowly has been hard with his driven mentality. He states, “It’s hard to turn back” [toward home], but after 2 weeks of easy movement, his running is in a gradual progression back toward normal.
Tracy Douglas is a 35-year-old runner from Colorado who also fell ill in mid-March. She works as a veterinarian in a busy clinic and some other staff were also becoming ill. The clinic acted quickly to protect their clients by keeping sick staff home, enforcing social distancing, and not allowing pet owners into the building. She went into quarantine at home with her fiance, and they notified the neighbors they had seen recently that they were sick. Tracy has asthma, a worrisome underlying condition.
Tracy immediately called her primary-care provider. She had a fever, but they pushed her off because she was young and at lower risk. She had to fight to get tested, and was finally able to when they agreed to test one person from their vet clinic. Tracy had the most predictable COVID-19 symptoms, so they gave her the test. Because of a testing backlog, she waited 7 days for her positive result.
After 6 days from the initial onset of symptoms, Tracy began to feel better, so much so that she thought she was coming out of it. Then on day 7 she crashed. This seems to be a classic pattern in COVID-19 patients where they turn the corner only to get worse again. For 4 days, Tracy was bedridden with a fever and shortness of breath. She called her doctor to figure out if she needed to go into the hospital. Like Jon, she had been sick before, but never like this.
Her doctor was concerned and said to go to the hospital if her symptoms got any worse. Being a “nerdy altitude runner,” Tracy was able to ride out her symptoms at home and monitor her oxygen saturation with a consumer monitor. Tracy’s fever broke, and she started to feel a little better, a day at a time. When I spoke to her 3 weeks after the end of her symptoms, she said she was feeling “pretty normal, but was still being conservative.”
I asked Tracy about her main takeaways. She thanked her neighbors for leaving meals on their doorstep and getting to see the good in humanity. She said, “For those runners who find themselves with the dreaded COVID-19 and even for those with the quarantine blues, know that in your deepest, darkest moments, there is light at the end of the tunnel. You will run again with clear lungs. You will find flow again.”
Both Jon and Tracy did incredible jobs of adjusting quickly when they realized they were sick to protect those around them. They were cared for by their communities near and far. And they are both being patient while being hungry to get back to doing what they love, running.
News and Updates
In this section, we summarize significant updates to relevant-to-runners recommendations by governments and organizations. We’ve also made in-text updates to this article that reflect them.
- Sunday, March 15 – The Centers for Disease Control and Prevention (CDC) have issued new nationwide guidance for large events and mass gatherings; this includes sporting events, conferences, festivals, and even weddings. The CDC is asking organizers and individuals to cancel or postpone any event of 50 people or more for the next 8 weeks (or about May 10). This new guidance is considered interim and subject to change as we learn more about COVID-19. Some of these precautions might feel over the top, and the goal of this guidance is not to keep things like schools or businesses closed indefinitely, but rather is geared toward events specifically. This is because events involve traveling and mingling between different family groups and communities and that is a considerable risk factor for spreading COVID-19. What does this mean for us, the running community? This is not a mandate (although there are state mandates that will continue to change and evolve), but it is something that race directors, running stores, groups runs, fat asses, and unofficial runs should be considering.
- Sunday, March 15 – Ultra-Endurance Sports Science & Medicine, a non-profit group of sports researchers and physicians, published an open letter to the endurance-sports community with its recommendations. To quote, “We now recommend that all organized endurance sporting events (group training, meetings, races, etc.) of more than 50 people (including organizers, athletes, spectators, volunteers, etc.) scheduled to occur before 15 June 2020, be immediately canceled or postponed. This is consistent with guidance released earlier today by the Centers for Disease Control and Prevention (CDC, 2020), except that we are recommending that events be canceled or postponed that are in the next 3 months rather than the next 2 months. If by 15 May 2020, the pandemic continues to grow, then an additional month of cancellation is warranted. Further cancellations should be considered on a rolling monthly basis with a two-month window depending on the current control of the pandemic. If the event involves fewer than 50 people and will still be held, participation by those using public transportation should be discouraged.”
- Monday, March 16 – Today, the U.S. White House recommended gathering no more than 10 people together and to practice strict social distancing in doing so.
- Saturday, April 4 – The Centers for Disease Control and Prevention (CDC) have now recommended mask and face-covering use in public.
Call for Comments (from Meghan)
This is a sensitive topic. We welcome you to constructively talk with each other in the comments section of this article, but please do so according to iRunFar’s comment policy. We additionally ask you to focus your comments on public health rather than politics. Comments not adhering to these requests are subject to redaction or removal. Thank you.
- Would you like to share a story about the COVID-19 pandemic in your local community and actions that are being taken to reduce its spread?
- If you are in a country where social-distancing and/or quarantine measures have been recommended or regulated, can you share how the experience is going?
[Editor’s Note: Thank you to Olivia Rissland and Eric Lee for advising in the development of this article.]
Resources
- CDC COVID-19 recommendations
- CDC educational video
- Johns Hopkins University Coronavirus Resource Center
- Flatten the COVID-19 Curve
- Joe Rogan Experience podcast excerpt with infectious disease expert Michael Osterholm
- iRunFar’s article “COVID-19 Race Updates: Cancellations, Postponements, and Races Still On”
- iRunFar’s article “Tips for Running During the COVID-19 Crisis (or Any Life-Altering Time)”
References
- Branswell, H. (2020, March 9). People ‘shed’ coronavirus early, but most likely not infectious after recovery. Retrieved from https://www.statnews.com/2020/03/09/people-shed-high-levels-of-coronavirus-study-finds-but-most-are-likely-not-infectious-after-recovery-begins/
- Riou, J., Hauser, A., Counotte, M. J., & Althaus, C. L. (2020). Adjusted age-specific case fatality ratio during the COVID-19 epidemic in Hubei, China, January and February 2020. doi: 10.1101/2020.03.04.20031104
- Tufekci, Z. (2020, February 27). Preparing for Coronavirus to Strike the U.S. Retrieved from https://blogs.scientificamerican.com/observations/preparing-for-coronavirus-to-strike-the-u-s/
- FlattenTheCurve.com. (2020, March 9). FlattenTheCurve: COVID19 Update & Guidance to Limit Spread. Retrieved from https://www.flattenthecurve.com/
- Coronavirus. (n.d.). Retrieved from https://www.who.int/health-topics/coronavirus
- Thomas, R. (n.d.). Covid-19, your community, and you – a data science perspective. Retrieved from https://www.fast.ai/2020/03/09/coronavirus/?fbclid=IwAR1PS-KLf74YFn_Tq8NyefndjEMfBS8ACnsgf2rBqMDVA8RlvHu7YpuDPkI
- Cascella, M., Rajinik, M., Cuomo, A., Dulebohn, S., & Di Napoli, R. (2020). Features, Evaluation and Treatment Coronavirus (COVID-19). StatsPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554776/
- Firth, S. (2020, March 5). Singapore: The Model for COVID-19 Response? Retrieved from https://www.medpagetoday.com/infectiousdisease/covid19/85254
- Baggaley, K. (2020, March 11). COVID-19 symptoms typically appear 5 days after infection. Retrieved from https://www.popsci.com/story/health/coronavirus-incubation-period-time-symptoms/
- Cool, J, and D Zappetti. “The Physiology of Stress.” Medical Student Well-Being, 5 Jan. 2019, pp. 1–15., doi: https://doi.org/10.1007/978-3-030-16558-1_.
- Van Doremalen, N, et al. “ Aerosol and Surface Stability of HCoV-19 (SARS-CoV-2) Compared to SARS-CoV-1.” NEJM Original Article, doi: https://doi.org/10.1101/2020.03.09.20033217.
- “2019-2020 U.S. Flu Season: Preliminary Burden Estimates.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 13 Mar. 2020, www.cdc.gov/flu/about/burden/preliminary-in-season-estimates.htm.
- Specht, Liz, and Ronald Katz. Simple Math Offers Alarming Answers about Covid-19, Health Care. 10 Mar. 2020, www.statnews.com/2020/03/10/simple-math-alarming-answers-covid-19/.
- Sanche, Steven, et al. “Early Release – High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2 – Volume 26, Number 7-July 2020 – Emerging Infectious Diseases Journal – CDC.”Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, wwwnc.cdc.gov/eid/article/26/7/20-0282_article.
- Mervosh, Sarah, et al. “See Which States and Cities Have Told Residents to Stay at Home.” The New York Times, The New York Times, 24 Mar. 2020, www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html.
- Greenhalgh, Trisha, et al. “Face Masks for the Public during the Covid-19 Crisis.” The BMJ, British Medical Journal Publishing Group, 9 Apr. 2020, www.bmj.com/content/369/bmj.m1435/li>
- Kushner, T. “SARS-CoV-2: Masks and Running.” Google, Google, docs.google.com/document/u/0/d/106lUZEmqbdToLVCD7BU-XkcCPvzIl8DgbrlNTZV3fo0/mobilebasic.

