We have a long-running joke around my household, “Oh, Corrine is just a handful of chocolate chips away from diabetes…” and although it’s not entirely true, I will acknowledge that I have a terrible sweet tooth and eat more sugar than I probably should. The ongoing joke planted a seed that turned to lingering fear, which ultimately prompted me to get blood work done. Sure enough, my fasting blood glucose was higher than I expected; 96 mg/dL (milligrams of glucose per deciliter of blood) to be precise. This is below what is considered ‘prediabetes’ (100 to 125mg/dL), but still it made me stop and think, Holy s^*t, am I going to get diabetes?!
Since then, I’ve started out on a knowledge quest of my own. Asking questions like, how important is my genetic history? How about my diet and lifestyle? How much gummy candy is too much gummy candy (read: so much fear!)? And how do all these things factors interact when it comes to influencing my blood glucose and insulin response on a day-to-day and long-term basis?
To get us started, there are two main types of diabetes; Type I and Type II. For our purposes, we’ll focus primarily on Type II diabetes. Type I diabetes is an autoimmune response that causes the body to stop producing the hormone insulin, and is most frequently diagnosed during childhood. People that have Type I diabetes have to take insulin (administered via an injection) in order to manage their blood glucose and if left untreated it can lead to serious health consequences including death. Type II diabetes is characterized by your body becoming less responsive to insulin, also referred to as insulin resistance. When this happens, you cannot properly use the glucose present in your blood for energy and your blood-glucose levels rise. This is important because your body not only uses insulin to access glucose in your blood to use it for energy but it also plays a key role in storing excess glucose as glycogen and fat to be used for energy later. In the early stages of Type II diabetes, or prediabetes, your pancreas is trying to get your cells to respond by producing more and more insulin, but over time gets worn down and stops functioning properly. When this happens, and your body can no longer keep up, your blood glucose (used interchangeably with blood sugar) rises as your body can no longer use insulin to keep your blood glucose within a normal range, 70 to 99mg/dL.
Lucky for us, a bunch of endurance junkies, for much of the past six or seven decades, exercise has largely been seen by both the scientific and medical communities as an effective means of lowering your risk of developing Type II diabetes. In fact, exercise is often prescribed as treatment and management for the disease (1). This is because short and long-term effects of exercise lead to weight loss/weight management, an increase in muscle mass, management of blood glucose by increasing its use via muscle contractions, and improved insulin sensitivity (7). One study showing the importance of not just weight management but lean muscle mass for fighting Type II diabetes risk found that for every 10% increase in skeletal muscle mass, an 11% reduction in insulin resistance and a 12% reduction in the prevalence of prediabetes was seen in their volunteers (8). In the graph below, you can see how glucose levels change during exercise, lowering insulin production and making more glucose available to your working muscles. In this sense, exercise over time is believed to make you more sensitive to insulin, or rather your body can utilize insulin more effectively. However, in recent years, there has been a growing concern that our increased reliance on processed foods–that are generally higher in added sugar and simple carbohydrates–and our increasingly sedentary lifestyle might be leading us toward a Type II diabetes epidemic of sorts. Alarmingly, in the Centers for Disease Control and Prevention’s 2017 diabetes report, they suggested one in 10 Americans has diabetes, and that 90 to 95% of those cases are Type II diabetes (2).
Because risk factors include being overweight, physical inactivity, poor dietary choices, and smoking, it seems odd that endurance sports could possibly be a contributing factor for Type II diabetes risk. In a study conducted by Marty Hoffman and Eswar Krishnan looking at medical issues amongst a wide range of 1,212 ultramarathon runners, only 0.7% reported having diabetes (3), far below the rates in the average population. So where does this fear come from?
Most of the arguments supporting this fear come from the link between high carbohydrate intake and chronically elevated blood sugar. See, when you eat carbohydrates, your digestive system breaks them down into sugar which can enter the blood, a la blood glucose. If you are chronically eating large quantities of carbohydrates, your body has to constantly work to manage that ever-shifting blood-glucose level while your muscles are not utilizing glucose for fuel. This is especially true of foods that have been classified as having a high glycemic index and glycemic load. The scale ranks carbohydrates from 0 to 100 based on how fast and by how much they cause your blood-glucose levels to rise after eating. Foods that rank high on this list are often processed like white rice, white flour products, refined breakfast cereals, sugar-sweetened beverages, my beloved gummy candies, and more. The fear is that as endurance athletes we may have a tendency to eat more of these products both on and off the trail, from our gels and love of coke to our pasta dinners and our “you ran today extra piece of pie.” That being said, this is a perceived fear and there are many of us on both sides. I’ve seen you with your pre-race sweet potatoes and I’ve seen myself shoveling candy directly into my face.
Like many things in life, timing is incredibly important. First, you should know that your blood glucose will naturally rise during and after exercise so that your muscles can get the blood sugar they need for energy. Blood-glucose levels will ebb and flow naturally but avoiding major sustained spikes and crashes in blood-glucose level is key. During exercise, blood glucose comes from a number of sources, including from the glycogen stored in your liver and muscles from carbohydrates you’ve ingested between your workouts and from the food/fluid you are taking in right before or during exercise. Our bodies are super smart and want to use the most readily available energy source. That being said, there is an ideal time and place for these easily digestible, quick-energy foods, and unfortunately it’s not all the time. The current recommendation from the World Health Organization is to limit your added sugar intake to roughly 5% or less of your daily caloric intake. So with an average caloric intake of 2,500 calories a day, that would limit me to no more than 31.25 grams of sugar per day or a little more than one serving of Swedish Fish. Not all, but many of us are probably toeing that line. As active people, we do have the ability to fudge that number a little bit, but likely need to tame what we are reaching for when it comes to food eaten away from our exercise. It’s important to note that although endurance athletes have a slightly higher recommendation for carbohydrate intake than the general population, the recommendation for sugar is the same.
A lot of concern was raised recently by a particular study that came out in 2016 that followed 10 athletic individuals for a week using a continuous glucose monitor (4). In this particular study, the individuals were classified as “subelite,” but there is no great standardized rationale for classifying individuals into groups in much of the literature. These volunteers in particular exercised on average six hours a week, had “average” to “excellent” VO2max values for their age and gender based on the general population, and had resting heart rates of less than 60 beats per minute. In general, they likely represent an average active population. What they found was that four of the 10 athletes spent more than 70% of the testing period with blood-glucose levels above 108 mg/dL. This result startled people, including researchers, because it was not what had been hypothesized at all. What was overlooked, however, was that the four athletes with the prediabetic blood-glucose levels had more differences than similarities. Two of the four athletes were the most active of the entire cohort during the testing week, while the other two were among the least active. One of the four under-consumed the recommended percentage of carbohydrates in their daily diet and still had high blood glucose, while another volunteer greatly overconsumed sugar by more than three times the recommended daily amount and still had completely normal fasted blood-glucose levels. Basically, there was a whole lot of variability with no definitive cause.
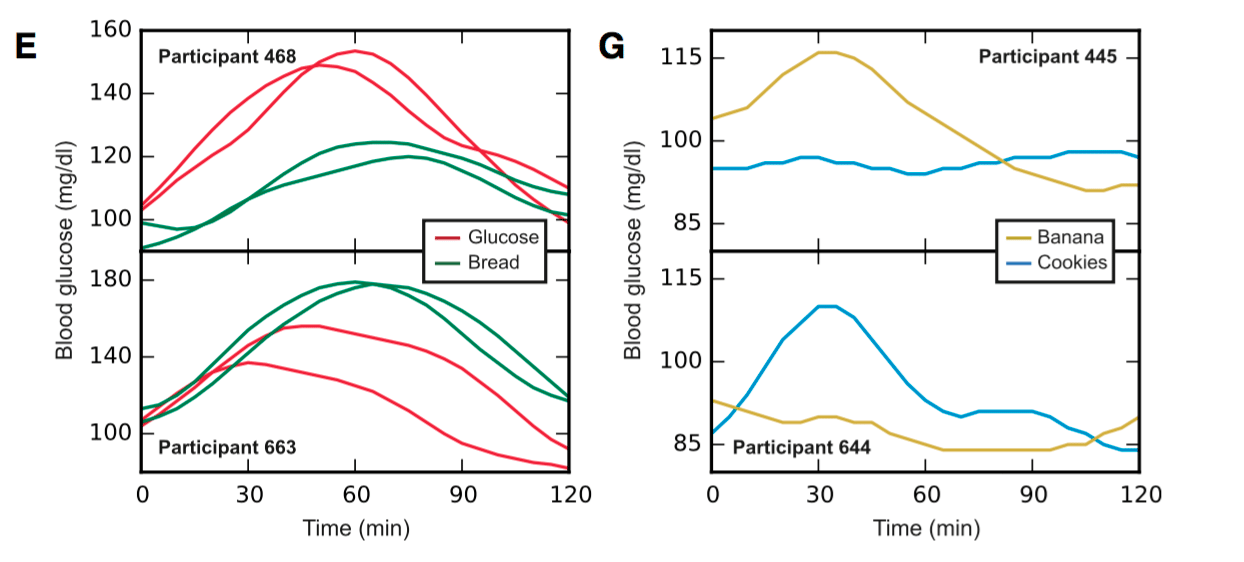
Having spent years on track to become the physiologist I had admired and looked up to, those same physiologists instilled in me the understanding that the correct answer in sports science is often, “it depends.” You see, what many overlook is the variability of individuals. Exercise physiology operates in shades of grey where there is rarely one right or wrong answer. Something might not work for everyone, and context is key. This is becoming better appreciated as our understanding of genetics develops. So, will consuming a balanced diet, a diet low in carbohydrates and high in fat, or one that utilizes periodized carbohydrates tip the scales for you? The correct answer is again, it depends. Like many diseases, the risk of developing Type II diabetes may largely depend on your genetics, which can predispose you for developing the disease. Additional factors to take into account are your training intensity and volume as well as what you chose to fuel your body with. A study highlighting this was conducted in Israel in 2015 monitoring 800 participants using continuous glucose monitors. They monitored the individual post-meal glycemic response and found that it varied greatly between individuals (8). Below you can see that a sample of the participants had different responses to the same foods, and that stresses the point that individuality should not be overlooked when drawing conclusions.
So what can you do?
- Avoid under fueling. We’ve all heard the adage, “calories in should equal calories out,” and there’s truth to that. Chronically starving your body of the calories it needs around intense exercise creates extra stress on our systems. Work stress, life stress, lack of sleep, and the stress that comes with the midterm I haven’t studied for all elevate your cortisol levels. Cortisol is a stress hormone that allows your body to function quickly and efficiently when threatened by increasing blood glucose into your bloodstream. This gives your brain the glucose it needs to act quickly and also increases the bioavailability of other substances to repair tissue from injury/inflammation/training stress. However, cortisol levels are supposed to drop off and return to baseline levels as your body resumes normal activity. Chronically high levels of cortisol disrupt the body’s normal functions, keeping your blood glucose high when your body does not need it.
- Eat enough fiber. This is especially true when it comes to soluble fiber (think oatmeal, sweet potatoes, citrus, and black or kidney beans) as it alters the rate of carbohydrate absorption. Slowing your body’s carbohydrate absorption slows your post-meal blood-glucose response and limits spikes in your blood glucose, which can help to regulate your insulin production (5).
- Match your carbohydrate intake to your training load. More and more scientific evidence is coming to the table in support of periodized carbohydrate intake. This means when workouts involve high-intensity or high volume, you should shoot for higher carbohydrate availability leading up to and during that day. Whereas, when your workouts are lower intensity, carbohydrate availability is less important, and you can reduce your carbohydrate intake. From a performance standpoint, you need both the adequate fuel stores for your race and metabolic flexibility so you can efficiently utilize multiple pathways when it comes to meeting your energy demands (6). Essentially, your body is never using only one energy pathway, which depends on a number of individual factors including intensity and your ability to utilize carbohydrates and fats at those different intensities. As you run longer and longer, it is especially advantageous to be able to utilize fat efficiently as well as carbohydrates. And if you are prone to gastro-intestinal distress, being able to take in slightly fewer grams of carbohydrates per hour can make the difference between that buckle or a DNF. By periodizing your carbohydrate intake, you can maximize your ability to utilize fat more efficiently as fuel while not compromising your ability to train at high intensities.
- Work with a sports dietitian to figure out what your individual dietary needs are. How you choose to fuel your body is as important as all the miles you run. As sports dietitian Dina Griffin would say, “we cannot outrun our crappy diets.”
So, am I going to get Type II diabetes? In all likelihood, no. Personally, thanks to a combination of good genetics, managing my stress, bringing my cortisol levels down, and matching my carbohydrate intake to my activity level, my fasted glucose levels are well within the normal range and will hopefully stay that way for years to come. And for you, my iRunFar audience, are you going to get diabetes? Truthfully, I don’t know. That’s between you, your genetics, and timing that extra piece of pie for your hard training day.
Call for Comments (from Meghan)
- Have you ever used a continuous glucose monitor to track your blood-glucose level over an extended period of time? If so, what did you find?
- Have you worked with a sports dietician to learn about your body’s specific needs and tailor your diet to them? What did you learn from that expert?
- Are you an ultrarunner with Type I or Type II diabetes? Would you care to share what you have learned about your body’s specific needs in the sport?
References
-
- Borghouts, L., & Keizer, H. (2000). Exercise and Insulin Sensitivity: A Review. International Journal of Sports Medicine, 21(1), 1-12.
- National Diabetes Statistics Report, 2017. (n.d.). Retrieved November 13, 2017, from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
- Hoffman, M. D., & Krishnan, E. (2014). Health and Exercise-Related Medical Issues among 1,212 Ultramarathon Runners: Baseline Findings from the Ultrarunners Longitudinal TRAcking (ULTRA) Study. PLoS ONE, 9(1). doi:10.1371/journal.pone.0083867
- Thomas, F., Pretty, C. G., Desaive, T., & Chase, J. G. (2016). Blood Glucose Levels of Subelite Athletes During 6 Days of Free Living. Journal of Diabetes Science and Technology, 10(6), 1335-1343. doi:10.1177/1932296816648344
- Ullrich, I. H., & Albrink, M. J. (1985). The effect of dietary fiber and other factors on insulin response: role in obesity. Journal of Pathology Toxicology and Oncology,5(6), 137-55.
- Burke, L. M. (2015). Re-Examining High-Fat Diets for Sports Performance: Did We Call the ‘Nail in the Coffin’ Too Soon? Sports Medicine, 45(S1), 33-49. doi:10.1007/s40279-015-0393-9
- Lebrun, C. (2011). Exercise and Type 2 Diabetes: American College of Sports Medicine and the American Diabetes Association: Joint Position Statement. Yearbook of Sports Medicine, 2011, 162-163. doi:10.1016/j.yspm.2011.03.038
- Zeevi, D. et al (2015). Personalized Nutrition by Prediction of Glycemic Responses. Cell,163(5), 1079-1094. doi:10.1016/j.cell.2015.11.001
- Srikanthan, P., & Karlamangla, A. (2011). Relative Muscle Mass is Inversely Associated with Insulin Resistance and Prediabetes. Findings from the Third National Health and Nutrition Examination Survey. Journal of Clinical Endocrinology & Metabolism. 96(9) 2898-2903. Doi:10.1210/jc.2011-0435