In this article, we’ll discuss:
- The epidemiology of anemia and iron deficiency in runners;
- Hemoglobin, iron, ferritin, and exercise performance;
- A couple of cases of anemia in female runners;
- Why running leads to chronic blood and iron loss;
- The symptoms and problems of iron excess; and
- Diagnosing the cause of anemia and treating it, with special guest, Rasmus Høeg, MD, Hematologist.
Case #1
I could not walk even four blocks to get to medical school–it was that bad. I called a cab. I could not breathe. If I walked, I was so short of breath that I felt like I might die.
This was crazy. I was a runner who regularly logged 70 to 80 miles a week without really getting winded. But in the last couple of weeks, my daily runs had been getting really tough. Then, I had barely been able to muster a jog, and if I did, I felt my heart pounding in my chest, even skipping beats. As much as I wanted to believe nothing was wrong, as much as I wanted to avoid going to see a doctor, I realized I could not live like this.
That afternoon, I went directly from class to the walk-in clinic of our medical school. The staff wondered if I was having a panic attack. Well sure, I was scared, but I didn’t think I was having a panic attack. My systolic blood pressure was in the 160s (normally it was in the 90s). Could anxiety do this, I wondered?
The doctor who saw me also wondered about my liver function since I was very yellow-colored. Eventually the blood tests came back and my hemoglobin was 5.8 g/dL (normal is 12.1 to 15.1 in women, as shown in Figure 6 below) and my hematocrit was 19% (normal is 37 to 48% for women). This was profound anemia; severe enough to get me admitted to the hospital. My treating doctors were incredulous, how could an otherwise healthy woman who had not been bleeding (I did not get my period at that time; so yes, you could say this was not healthy) become so severely anemic?
Anemia and Iron Deficiency: Background and Prevalence
So what is anemia? Simply put, it is a condition in which you don’t have enough healthy red blood cells to carry adequate oxygen to the body’s tissues. It can be caused by a number of things including blood loss, lack of iron, lack of B12 or folate, destruction of red blood cells (called hemolysis), or failure of the bone marrow to produce enough blood cells. However, in runners and in the general population, the most common cause is iron deficiency.
Iron deficiency is when the body has inadequate iron. Men typically have 4g of iron in the body while females have 2.5g. Iron deficiency can be diagnosed when serum ferritin is less than 30 ng/mL (Goodnough, 2010), though others would argue one can be symptomatic at levels of less than 50ng/mL. In fact, the diagnosis of iron deficiency is not clear-cut and if a person’s symptoms improve with iron supplementation, they can still be diagnosed with iron deficiency (Schrier, 2018).
[Author’s Note: A number of different laboratory tests, like tests for serum ferritin described above, will be mentioned in this article and their definitions can be found in the Appendix at the end.]
Iron’s largest role is in making and supporting red blood cells (Figure 1), but is also involved the production of neurotransmitters and the protection and function of neurons. It is involved in numerous other biochemical reactions, too numerous to name, and likely more than have been discovered. The most common symptoms of iron deficiency are fatigue, depressed mood, decreased cognitive function, and decreased exercise capacity. On average in healthy adults, men lose 1mg/day of iron and females 2mg/day due to the normal ‘sloughing off’ of the gastrointestinal (GI) tract and also due to blood loss in menstruating females (Clénin, 2017).
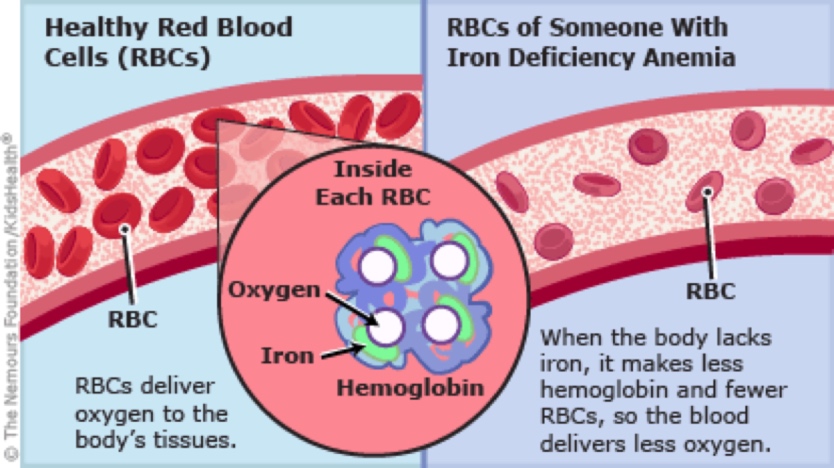
Figure 1. The role of iron in the hemoglobin molecule and the number of red blood cells in a healthy person’s artery versus an anemic person’s artery. Image courtesy of Kidshealth.org/en/parents/anemia.html.
A tricky thing to understand is that lack of iron can cause anemia and anemia (due to blood loss) can cause iron deficiency. The former is because if you don’t have enough iron, you can’t make enough red blood cells. The latter is because, if you lose blood, you lose a lot of iron with it. (Again, see the iron in the red blood cell in Figure 1.) So someone who has been bleeding and has inadequate iron intake has double the risk factors for both anemia and iron deficiency.
Importantly to athletes, both anemia and iron deficiency (alone or together) can cause decreased exercise performance and athletes, particularly runners, are at relatively high risk of of both.
Specifically, with regard to anemia, one small study found anemia in 87.5% of triathletes and 31.3% of runners (Coates, 2017). One study found iron-deficiency anemia in 35% of female distance runners and iron deficiency in 50% (Ostojic, 2008). Another study of collegiate cross-country runners found anemia in 2.2% of females and 1.2% of males, but iron deficiency in 33.1% of females and 3.1% of males (Parks, 2017). A third study found an even higher rate in female distance runners of 35% with anemia and 50% with iron deficiency (Clement, 1982). These studies clearly demonstrate that you can be iron deficient without being anemic and that females are at greater risk of both.
Just to put these numbers in perspective, the prevalence of anemia in the United States is estimated to be 5.6% (Le, 2016), which is mostly due to iron deficiency. The prevalence is higher in women (7.6%) than in men (3.5%), believed to be mostly due to menstrual-blood loss. However, these large population studies do not go into enough detail to prove the cause. The prevalence of anemia worldwide is approximately 24%, sadly highest in preschool-age children (60% of children under five years of age are anemic in Africa), and the major cause is insufficient dietary iron (deBenoist, 2008; Semedo, 2014).
Hemoglobin, Anemia, and Exercise Performance
Anemia greatly impacts running performance because inadequate oxygen is delivered to the muscles, including that all-important heart muscle. Specifically, a decrease in hemoglobin level of 1 g/kg was associated with a decrease in VO2 max of 4.4 mL/kg/min (for males it is 4.2 mL/kg/min, and females it is 4.6 mL/mg/min) (Otto, 2013). This is also shown in figures 2 and 3, which show the relationship between hemoglobin level and VO2 max and oxygen uptake into muscles, respectively.

Figure 2. Change in hemoglobin (shown as [Hb]) versus change in VO2 max. Hemodilution is blood letting. Image courtesy of Otto JM, Montgomery HE, Richards T. Haemoglobin concentration and mass as determinants of exercise performance and of surgical outcome. Extrem Physiol Med. 2013;2(1):33. Published 2013 Nov 26. doi:10.1186/2046-7648-2-33.

Figure 3. Hemoglobin level and its relation to oxygen uptake into the muscles in males and females. Image courtesy of Otto JM, Montgomery HE, Richards T. Haemoglobin concentration and mass as determinants of exercise performance and of surgical outcome. Extrem Physiol Med. 2013;2(1):33. Published 2013 Nov 26. doi:10.1186/2046-7648-2-33.
Iron Deficiency
There are three generally accepted stages of iron-deficiency anemia as defined by Mercer, 2005:
- Decreased ferritin but normal iron and hemoglobin;
- Iron deficiency, which can be seen in decreased iron level, decreased transferrin (a blood protein that binds to iron and transports it throughout the body) saturation, and/or an increase in total iron binding capacity (TIBC); and
- Anemia
Iron deficiency also affects exercise performance. Iron deficiency without anemia alone can cause a decrease in VO2 max (Figure 4) (Martens, 2018). This study also showed an increased rate of mortality in patients with iron deficiency, but given they had heart failure, this may not apply to the general population.

Figure 4. Iron deficiency without anemia can lower VO2 max more than anemia without iron deficiency. Image courtesy of Martens P, Nijst P, Verbrugge FH, Smeets K, Dupont M, Mullens W. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol. 2018;73:115–23.
Iron supplementation in pill form has been found to increase aerobic capacity (specifically VO2 max) in non-anemic but iron-deficient runners (Burden, 2015). Gravican et al. in 2014 also showed intravenous (IV) iron supplementation in runners with low ferritin or iron at the low end of normal caused an increase in VO2 max following supplementation. (Please note that IV infusion is on the World Anti-Doping Agengy [WADA] list of prohibited methods at a certain volume per unit of time.)
Additionally, with regard to IV iron treatment, even if your hemoglobin, iron, and ferritin are normal, IV iron treatment over six weeks was associated with improved mood, decreased fatigue symptoms, and improved 10 x 400-meter times (at two weeks) (Woods, 2014). This study does raise questions in my mind about what the true ‘normal’ level of iron and ferritin are.
Figure 5 below demonstrates nicely the relationship between ferritin levels and symptoms of iron deficiency. (More symptoms have a higher number on the Y axis.) When the patient took iron supplementation, her ferritin rose and symptoms disappeared without any change in hemoglobin or evidence of anemia. For more details about this study and another case example, see Soppi, 2018. Keep in mind that anecdotal reports are not as strong of evidence as a large study with a control group.
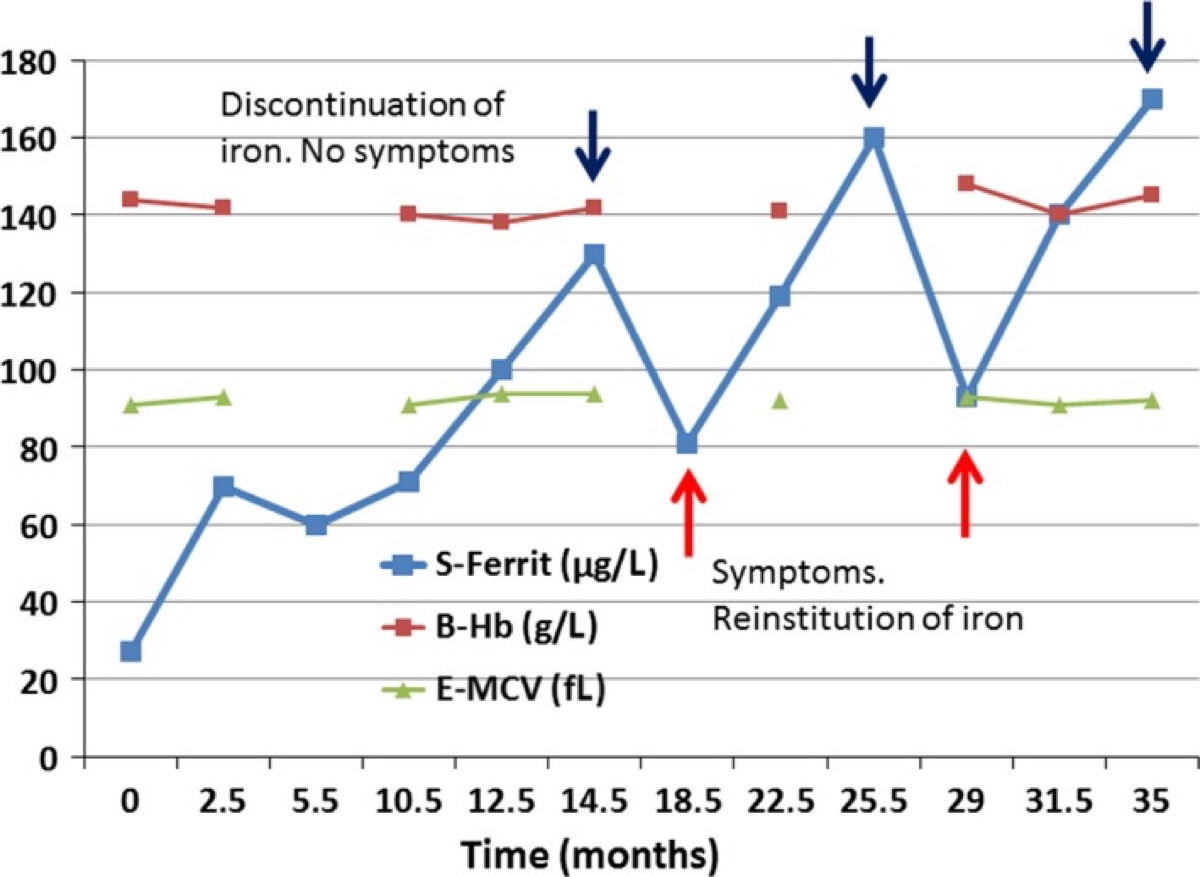
Figure 5. The relationship between ferritin, hemoglobin, hematocrit, iron supplementation, and “symptoms” in a patient. S-Ferrit is serum ferritin, B-Hb is blood hemoglobin, E-MCV is estimated mean corpuscular volume (or red blood cell size). Image courtesy of Soppi ET. Iron deficiency without anemia – a clinical challenge. Clin Case Rep. 2018;6(6):1082-1086. Published 2018 Apr 17. doi:10.1002/ccr3.1529.
The Figure 5 evidence supports that athletes with fatigue symptoms, decreasing performance, shortness of breath, and more should thus not only check hemoglobin and hematocrit (and the rest of the blood counts) but also iron and ferritin levels. Given the above epidemiological data, there are likely many athletes in which iron deficiency is overlooked and not diagnosed when they are found not to be anemic.
Why Runners Get Anemic and/or Iron Deficient
Runners go through their red blood cells, and thus also their iron, very quickly. The average blood cell will survive around 120 days in the average (sedentary) adult, but survives only about 74 days in an average runner (Weight, 1991). This is presumably due to the combination of blood loss and mechanical stress causing red blood cell breakdown, as discussed shortly. And that is the great ‘irony’ (so to speak): runners who need adequate hemoglobin to run are very prone to developing anemia. Just days after the resumption of an exercise program, iron stores significantly decrease (Terink, 2018). Despite iron continuously being lost during exercise, there is no innate mechanism to replace it, so sufficient iron must either come through the diet or supplementation (Ottomano, 2012).
The main ways the body uses and loses blood and iron during running are:
- GI bleeding;
- Urinary-tract bleeding;
- Hemolysis or the rupture of red blood cells;
- Sweating;
- Inflammation via an increase in the hormone hepcidin; and
- Travel to higher altitude.
Additional ways runners can have a sudden drop in hemoglobin without bleeding or iron deficiency are:
- Increase in plasma volume (pseudoanemia) associated with increased training and pregnancy, and
- Descent from altitude or space.
Let’s discuss these concepts in more detail.
GI-Tract Blood Loss
Bleeding into the stool that is not visible appears to be very common among distance runners. In fact, 85% of participating research subjects in one 100-mile race were found to have “occult” (or invisible) blood in their stool after the finish (Baska, 1990). The one study I could find that looked at the marathon distance (McCabe, 1986) found 23% of participating finishers to have detectable (though not necessarily visible) blood in their stool following the race. Bleeding from the GI tract is believed to either be caused by decreased blood flow to the GI tract or increased acidity directly breaking down the GI tract and causing bleeding (Choi, 2006). It is most likely a combination of both. Additionally, given non-athletes lose 1 to 2mg/day of iron through the sloughing off of their GI tract (Clénin, 2017), I wonder if athletes lose more via this route, though am unable to find a study that has been done to determine amount of iron loss through the stool without any blood in athletes.
Urinary-Tract Blood Loss
In terms of losing iron through urine, there are a number of things that may occur including mechanical trauma in the kidney or bladder wall in addition to breakdown of red blood cells in the bloodstream (hemolysis), which leads to loss of hemoglobin via the kidney (Ottomano, 2012, De DeRuisseau KC, 2002; McInnis, 1998). McInnis in 1998 found that intense exercise was more likely to cause blood in the urine since kidney blood flow is decreased proportionally to exercise intensity, similar to in the GI tract. I have had a number of runners report to me that they have actually seen blood in their urine following a race or intense training session, which is called march hematuria. If the urine is red, this is likely due to an irritated, bleeding small blood vessel and, if the urine is dark, this is more likely the breakdown products of red blood cells and/or muscle cells.
Hemolysis
The breakdown of red blood cells appears to occur in many forms of exercise (Ottomano, 2012), but occurs to a fourfold greater extent in running than in cycling (Telford, 2003). The discrepancy between running and cycling is believed to be due to foot strike (Telford, 2003). Indeed, runners wearing more cushioned shoes have less hemolysis (Dressendorfer, 1992). Interestingly, Miller and colleagues in 1988 found significantly greater changes in serum haptoglobin and plasma free Hb levels (both are markers of hemolysis) during downhill running, when compared to an uphill run of equivalent duration and gradient. (Just to be clear, foot-strike hemolysis or the breakdown of blood cells related to foot strike does not occur in the feet, but is a result of the landing impact on the body.)
Sweat-Related Iron Loss
Iron is a constituent of sweat. Sweat iron loss via sweat is estimated to occur at 1% and 3% recommended daily intake of iron per two hours of exercise for women and men, respectively (DeRuisseau KC, 2002).
Hepcidin and Inflammation
Systemic inflammation related to intense training or overtraining and/or muscle breakdown can actually lower iron levels via a hormone called hepcidin (Roecker, 2005; Peeling, 2009). There is a direct relationship between the initiation of an exercise program, decrease in iron level, and increase in hepcidin levels (Terink, 2018). Hepcidin signals for macrophages (immune cells) and liver cells to hide iron away inside of them and also causes decreased absorption of iron from the GI tract. It is important to note that when hepcidin is elevated, ferritin will also be elevated. So, if your ferritin is low or normal, your anemia is likely not due to inflammation.
Travel to Altitude
When people travel to higher altitude, they increase their red blood cell production, thus requiring more iron. Please see Corrine Malcolm’s excellent article on this topic!
Increased Plasma Volume
Increased plasma volume induced by training also tends to lower hemoglobin and hematoctrit. This is called pseudoanemia because it is simply due to an increased amount of plasma, but your actual number of red blood cells stays the same.
Descent from Altitude
Pertinent to many runners is the fact that when you descend from altitude, there is a selective breakdown (hemolysis) of young red blood cells (Chang, 2009). Perhaps less pertinent to runners is that this same effect occurs following return from space flight (Franco, 2009; Rice, 2001; Chang, 2009; Alfrey, 1997). When you descend from altitude (or space), the body is somehow able to sense there are too many red blood cells in the blood vessels (this is called plethora) and selectively kills the young red blood cells. (The exact mechanism, as far as I can find, has not been described.) The young blood cells survive the longest, so it makes sense to get rid of those first. It must have been an evolutionary adaptation for stopping the blood from getting too thick, which can cause strokes or heart attacks via clotting. This may result in normal or even high iron levels with low-normal or lower-than-previous hemoglobin levels.
Expected Sex Differences and Age-Related Changes in Hemoglobin Levels
The normal hemoglobin level is approximately 12 g/dl in women and 13g/dl in men (Murphy, 2014). This appears to be related to sex hormone levels, perhaps most importantly testosterone (Roy, 2017). Testosterone supplementation can actually reverse or ‘cure’ anemia in aging men (Roy, 2017), though the reason it does this is not yet clear and, further, testosterone supplementation is banned by WADA. As you will note, in the table of normals by age in Figure 8, men’s and women’s hemoglobin levels tend to decline with age, but more so for men. Of note, normal hemoglobin levels in boys and girls before puberty is the same and it approaches the same level again in late life.
Despite having lower hemoglobin levels, women are better able to take oxygen up into their muscles due to improved mitochondrial use of oxygen (or respiration) (Cardinale, 2018).

Figure 6. Normal hemoglobin levels by sex and age. Image courtesy of Disabled-world.com/calculators-charts/hemoglobin-iron.php.

Figure 7. Normal hemoglobin levels by sex and age. White circles are females. Image courtesy of Mahlknecht, U. & Kaiser, S. (2010). Age-related changes in peripheral blood counts in humans. Experimental and Therapeutic Medicine, 1, 1019-1025.
Case #2
In the fall of 2017, Kaci Lickteig sustained a pelvic stress fracture and did not run for four months. Prior to resuming her training program, she had her hemoglobin tested and it was normal at 14.3 g/dL. Then, over the course of two months, she gradually started to train and build back her fitness and noticed something was off.
As Kaci explained on her blog: “I started to notice I wasn’t feeling quite right on some of my runs. I felt like my effort was more labored than it should be. I kept telling myself, Oh it’s just because you are getting back into shape. This is normal. Then it happened. I was running one of my standard routes that I have done a bazillion times. As I was running up the slight hill my legs felt like they were completely gassed and in a lactic acid state and my heart started feeling like it was beating out of my chest. I had to stop at the top and regroup. This feeling was a red flag to me. I knew from the past and having been anemic off and on that these were anemia signs and symptoms.”
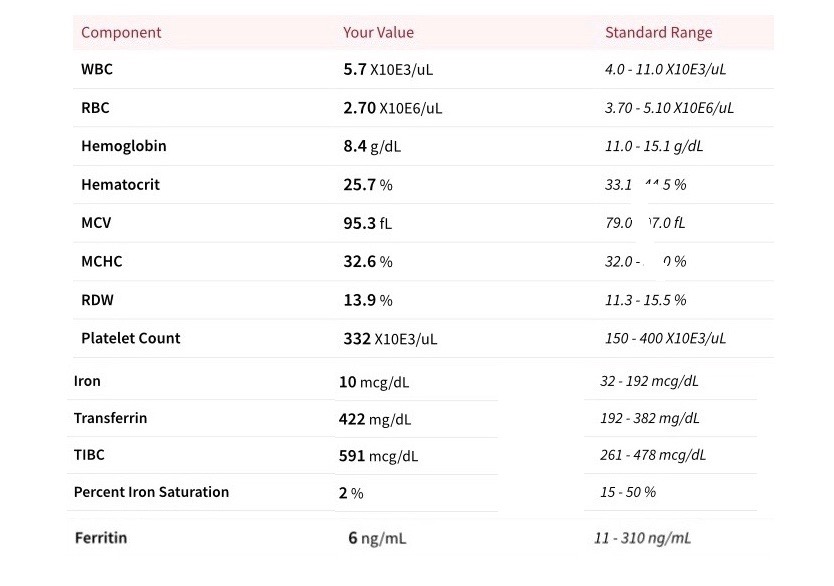
These labs exemplify a classic case of iron-deficiency anemia. Kaci was kind enough to agree to be interviewed for this article.
She describes, “I had not been running (prior to January 22nd) due to my injury and was only lifting weights (no legs involved) and cross training on the bike and Arc Trainer (non-impact activities). Then, starting on January 26, I [tried] to incorporate running. I tested a couple short runs outside and it was too painful yet. So, I was put in physical therapy and could run on the AlterG treadmill starting at 65% of my body weight. In the next couple of months, I increased how much body weight I was able to run at and then tested running outside again.
“It wasn’t until the beginning of March that I was running more consistently. I started to feel like my runs were becoming extremely difficult. I was running, to my standards, extremely slow to start out and even slower as the days went on. Not intentional by any means. I was not in shape, but this was a much different feeling, like I had been sprinting all out. The pain was substantial, like my body was building up lactic acid. My heart would pound so hard I could see it if I looked down at my chest and my breathing was heavy and labored.”
Reading about her experience from home, I had wondered if this sudden development of anemia was related to menstrual-blood loss (just as my doctors had falsely assumed when I was hospitalized for anemia), but this was incorrect. Though she had been getting her period prior to January 22nd, she did not get her period during the two months she developed her anemia. She also added, “During my injury, I stopped taking my iron-pill supplement as I didn’t think I would need it.” She had initially developed iron-deficiency anemia in high school during a self-described time of “under-eating and overtraining.” So this is the case of a young woman with sudden-onset anemia following a return to running, but not due to menstruation.
This left me wondering how often iron deficiency and iron-deficiency anemia in female runners are actually not related to menstruation. Could the increased losses of iron, building up of tissues, and microscopic blood loss be the whole explanation? I wondered if a lack of iron or anemia could, via hormone-level changes, stop a woman from getting her period. I did a thorough PubMed search for these questions and could not come up with any solid scientific research to answer them. However, female runners who do not eat red meat appear to be at remarkably high risk of developing iron deficiency and iron-deficiency anemia. I believe it is a combination of the above-listed factors and, if a female is also menstruating, this would be expected to put her at even higher risk.
Kaci’s primary doctor suspected her anemia was due to foot-strike hemolysis. However, I note that she did not have any lab testing for hemolysis so this can’t be confirmed. Kaci has made the following changes to her diet (and was previously a self-proclaimed “rut eater” who tended to eat the same things day after day) and also did not eat red meat:
- Eating red meat at least two to three times a week;
- Using a cast-iron skillet;
- Changing her diet to include more iron-rich foods such as Cream of Wheat, spinach, black beans, and fortified foods; and
- Taking an iron supplement twice a day per doctor’s recommendation of ferrous sulfate (325 mg) and vitamin C.
Kaci’s most current labs, from just a couple weeks ago, look greatly improved, however they still show mild iron deficiency:
- Ferritin (ng/mL) – 17 (normal is 10-154)
- Hemoglobin (g/dL) – 12.9 (normal is 2-18)
- Iron (ug/dL) – 37* (normal is 40-190)
- TIBC (ug/dL) – 510* (normal is 250-450)
- Transferrin Saturation (%) – 7* (normal is 11-50)
- Red blood cells (x10E6/µL) – 4.3 (normal is 3.9-5.2)
- Hematocrit (%) – 45.4* (normal is 1-44.9)
- MCV (fL) – 107* (normal is 4-94.8)
- MCHC (g/dL) – 28.4* (normal is 5-36)
- RDW (%) – 17.8* (normal is 5-14.3)
- Platelets (thousands/uL) – 271 (normal is 140-440)
- Vitamin B12 – 1377 pg/m
*indicates outside of the normal range
Here is my interpretation of her labs: Low ferritin, iron, and transferrin saturation; MCHC; and high TIBC all suggest continued albeit more mild iron deficiency. Her hemoglobin is within normal, though she did admit to being very dehydrated when she took the labs, which explains her elevated hematocrit, and may have falsely made her hemoglobin level look normal. Her elevated MCV and RDW suggest she is making new blood cells rapidly (likely to compensate for the recent anemia) given her B12 level was normal. She appears to be on the road to recovery, but it’s recommended that she continue with the iron supplementation and dietary changes and have her labs rechecked again in six months.
[Author’s Note: Thank you to Kaci for being so open and sharing her story with us!]
Current Recommendations on Iron Supplementation
The current position statement from the International Olympic Committee (Maughan, 2018) regarding iron and the high-performance athlete includes the following:
- “Suboptimal iron status may result from limited iron intake, poor bioavailability and/or inadequate energy intake, or excess iron need due to rapid growth, high-altitude training, menstrual blood loss, foot-strike haemolysis, or excess losses in sweat, urine or faeces (Thomas, 2016).”
- “Several measures performed simultaneously provide the best assessment and determine the stage of deficiency. Recommended measures: serum ferritin, transferrin saturation, serum iron, transferrin receptor, zinc protoporphyrin, haemoglobin, haematocrit and mean corpuscular volume (Gibson, 2005).”
- “Athletes who do not maintain adequate iron status may need supplemental iron at doses greater than their RDA [recommended daily allowance] (ie, >18 mg/day for women and >8 mg/day for men). Athletes with iron deficiency require clinical follow-up, which may include supplementation with larger doses of oral iron supplementation along with improved dietary iron intake (Thomas, 2016).”
- “High dose iron supplementation should not be taken unless iron deficiency is present.”
Anemia Treatment
Before you embark on taking supplemental iron, I do recommend both men and women have their complete blood count (CBC) and iron panel tested. However, eating a diet rich in iron is likely a safe thing for runners to do.
For anyone who tends to be iron deficient, it is helpful to know which foods are rich in iron. These foods include red meat, shellfish, spinach, liver, legumes, pumpkin seeds, sesame seeds, quinoa, turkey, broccoli, tofu, dark chocolate, oats, sesame seeds, coconut milk, and fortified cereals.
If you are found to have any of the stages of iron deficiency, you may also choose to supplement with a maximum of 325 mg ferrous sulfate three times a day. IV iron can also be considered in more severe cases of iron-deficiency anemia.
However, when it comes to iron absorption, there is a big difference between heme and non-heme iron absorption. Heme iron, or actual hemoglobin (in other words, blood), only comes from eating animals and has an absorption rate as high as 35% while non-heme iron (all non-animal forms of iron) has an absorption rate as low as 1%. However, consuming heme iron has been linked to an increased risk in colon cancer (Bastide, 2015), breast cancer (Diallo, 2016), and all-cause mortality (Etemadi, 2017).
If you do not wish to eat meat or heme iron, you can also increase your iron absorption by eating vitamin-C-rich foods or taking vitamin C when eating (which increases iron absorption by up to 300%!) However, vitamin C actually converts iron into a more potent pro-oxidant (argh, nutritional medicine is just never simple), but if you are severely iron deficient, I would still agree with adding vitamin C to increase absorption. Avoid drinking coffee (I guess it’s the phenolic acid and not the caffeine) and tea with your meals (which can decrease absorption by up to 90%). Consider cooking in a cast-iron pan, which can transfer two to three times more iron to the prepared food than conventional cookware. Finally, antacid use and h. pylori bacterial infection, and any form of chronic diarrhea, can significantly reduce the absorption of iron.
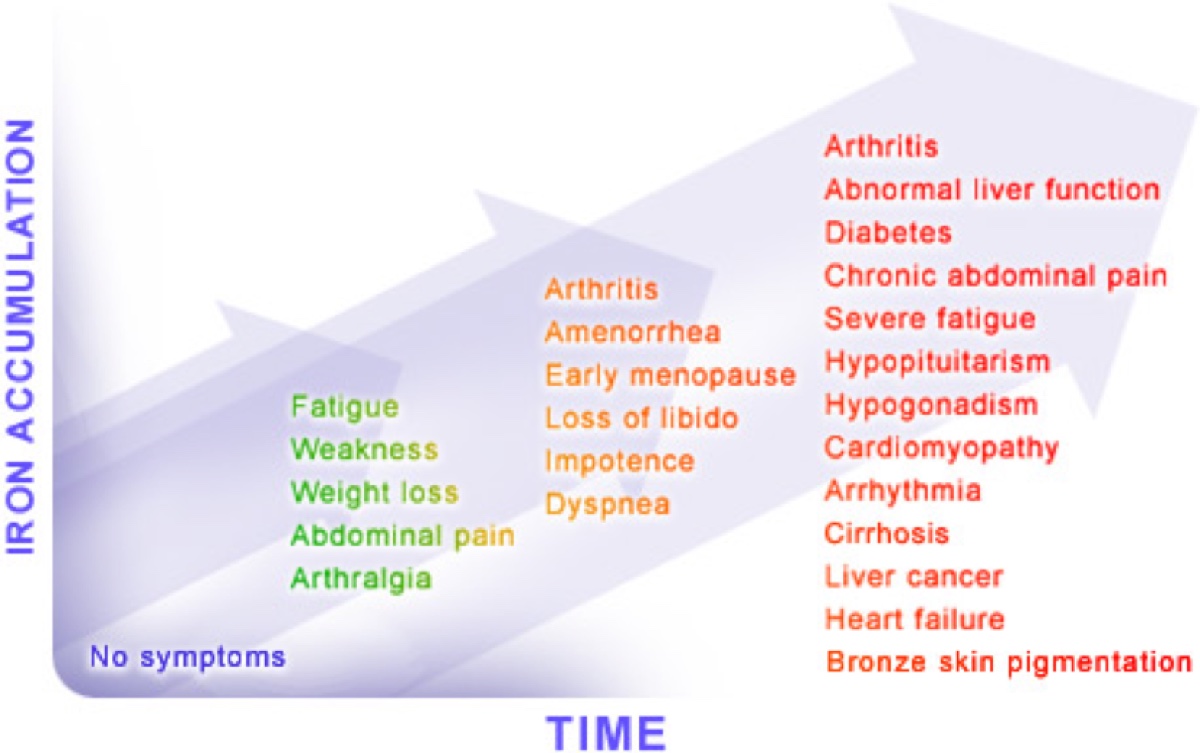
Iron Excess or Overload
But while iron for the iron-deficient person is good, too much iron for the non-iron deficient has serious risks. An interesting thing about iron that sets it apart from most other minerals and vitamins is that the human body has no built-in, automatic mechanism of eliminating it, unless you bleed regularly. Iron supplementation in those with already-adequate iron stores can result in symptoms that may begin with vomiting, diarrhea, and abdominal pain, and progress to hemochromatosis (systemic disease caused by iron overload) and liver failure (Mettler, 2010). Iron, rather than being an anti-oxidant is actually a pro-oxidant, meaning it causes tissue destruction, can cause diabetes, heart disease, bronzing of the skin, and many other disorders when at a high-enough levels. Mice with iron overload have also been found to have decreased exercise performance, and it was felt iron overload may play a significant role in skeletal muscle atrophy (Reardon, 2009). Iron excess has been found in 19 out of 127 (15.0%) male runners and 2 out of 43 in females (4.7%) (Mettler, 2010), which sounds to be related to excessive/unnecessary supplementation.
Case #1 Continued
While still in the hospital, I was diagnosed with both celiac disease (a surprisingly common cause of iron-deficiency anemia) and clostridium difficile (a bacterial infection, rare at that time, which causes loose stools and malabsorption). I gave up wheat and was treated with the antibiotic metronidazole (Flagyl). A few weeks after being discharged from the hospital, I underwent an endoscopy and colonoscopy (both of which were normal) to determine if there was any obvious GI bleeding occurring. When a bone-marrow biopsy was recommended by my hematologist, I suggested I try eating liver for dinner every night for one week and come back. After that one week, my hemoglobin was normal again. Granted it had been steadily rising prior to that, but it did not come up into the normal range despite weeks of iron supplementation until I changed my diet. This has always intrigued me and, when writing this article, I finally may have found the explanation. (See heme versus non-heme iron above.) Since this hospitalization, I have had my hemoglobin and hematocrit checked a few times and they have always been normal, however, I have not had my iron tested. A couple of weeks ago while beginning to do research for this article, I started to take 325mg of ferrous sulfate twice a day and I have to say I am pleasantly surprised with my running times and overall energy level. Since I am a pesco-vegetarian with a pretty demanding training schedule, I now realize how high of risk I am for iron deficiency. Now I just need to make an appointment to get my iron labs tested so that I practice what I preach!
Anemia-Treatment Discussion with a Hemotologist
At this time, I would like to bring in my ‘in-house’ (he is my husband) hematologist, Rasmus Høeg, MD, Assistant Professor of Hematology and Oncology at UC Davis School of Medicine.
iRunFar: Can you comment on Kaci’s labs and whether or not these are indicative of hemolysis? To me these look like typical iron-deficiency labs and, given she did not menstruate between the time of the two labs, could you postulate what the most likely cause would be? Should she have additional testing? Do you recommend that athletes like Kaci who tend to get iron-deficiency anemia take iron supplements to prevent its development (even if they are not currently anemic)?
Rasmus Høeg: I agree that the labs are all very suggestive of iron deficiency. I don’t know what else it could be. Foot-strike hemolysis or hemolysis in general would not be expected to cause that degree of iron-deficiency anemia so quickly (though hemolysis lab tests should be ordered if this is suspected). Now, the next question in a case of iron-deficiency is always, “Where did all the iron (blood) go?” Doctors will often blame heavy periods or, in the absence of heavy periods, worry about GI or genitourinary blood loss. As you know from your own case, the next step is often to order a colonoscopy and/or upper endoscopy.
Kaci’s sudden development of anemia is unusual. But of course anemias don’t read textbooks. I suspect that she was living with a mild degree of iron deficiency during her more sedentary months. In other words, she was able to produce enough hemoglobin to stay non-anemic. However, once she started exercising and her demand for hemoglobin increased, she was unable to keep up with production. Honestly, elite athletes like Kaci do not really adhere to normal rules of medicine.
I think it makes sense for Kaci to take supplemental iron, at least if she can tolerate it. If she were my patient, I would order a CBC with iron studies every so often (maybe every six months) and see where things are at. By the way, during her more serious iron deficiency, some doctors would have considered IV iron as a treatment of her anemia.
iRunFar: Is there an indication for using IV iron to treat iron-deficiency anemia in your mind and, if so, what?
Rasmus Høeg: The usual indication for IV iron is significant iron deficiency in a patient who is unable to tolerate oral iron. But there is no clear cutoff for when to give IV iron. Most patients do not like taking oral iron. For example, few patients are able to take the full dose of 325 mg ferrous sulfate three times daily. So what do you do with a patient who has some improvement with oral iron, but who is still anemic and is unable to increase her oral dose?
IV iron can sometimes work very quickly and is very effective. I think one reason IV iron is not used more frequently is that it carries the stigma of being associated with nasty infusion reactions. It is true that the ‘old’ form of IV iron, called iron dextran, can cause an anaphylactic reaction when it is infused. It requires that you give a tiny test dose and watch the patient for a while, before giving the full dose. Stuff like that worries doctors, of course.
There are many new formulations of IV iron that have almost no infusion reaction. But then some insurance companies will insist you try iron dextran first etc. In fact, like all IV medications, there is the added insurance hassle that doctors don’t like to deal with. All in all, IV iron takes a little bit of getting used to from the doctor’s standpoint.
If I were a patient/athlete being offered IV iron for iron deficiency, I would definitely say yes.
iRunFar: Are you aware of anyone besides those with the disease hereditary hemochromatosis (a disease where too much iron is absorbed and stored) developing iron excess through diet alone and without taking supplements?
Rasmus Høeg: First of all, most patients who develop significant iron overload do so because of frequent blood transfusions. Blood, as you know, has a lot of iron in it. If a person has a disease with a need for ongoing blood transfusions, iron overload will invariably develop. This can be a huge problem and these patients should avoid all iron supplementation.
Good question about hemochromatosis. The problem is that hereditary hemochromatosis comes in various forms. There are two main hemochromatosis mutations that are passed down in families and they can combine in various ways to increase the risk of clinical iron overload. Something like 10% of people with European ancestry are carriers of hemochromatosis and are at a higher (yet still very low) risk of developing clinical iron overload. If such a low-risk person does develop iron overload despite all odds, you would wonder if this was caused by excessive iron supplementation.
I personally think a person without any hemochromatosis gene would have to be pretty zealous with his iron supplementation to develop iron overload. And, yes, that zealot would have to be a man, because men generally develop iron overload much more frequently than women due to their lack of periods.
Easily available gene panels like 23andMe test for hemochromatosis as well as carrier status, by the way.
iRunFar: Do you think the recommended daily intake of iron should be higher for runners than sedentary adults?
Rasmus Høeg: For a runner without any history of iron deficiency, I would not recommend taking supplemental iron. People hate taking iron. It has a lot of GI side effects, such as abdominal pain and diarrhea or constipation. Some supplements are better tolerated, sometimes because the amount of iron in it is very low, and sometimes because everyone tolerates things a little differently. A few exceptions, in which I think taking ‘preemptive’ iron are menstruating or pregnant women, or people moving to altitude to train. These situations lead to a higher demand for iron.
A related question might then be, who should have a CBC and iron studies checked? I think any unexplained drop in performance, any symptoms of anemia, pregnancy (which also has an increased prevalence of both iron deficiency and anemia), heavy menses etc. would justify these tests, for reasons you have outlines above.
iRunFar: Do you have any tips for someone who would like to get their hemoglobin into the upper end of normal if their iron stores are full/normal?
Rasmus Høeg: No specific tips. In fact, most athletes will have hemoglobin concentrations in the lower end of normal due to a higher plasma volume. So we should not expect to see high levels of hemoglobin in most athletes. Of course, altitude training and substitutes such as altitude huts and tents can produce the effect in some runners. And, as we know from all the doping we have seen in professional endurance sports, erythropoietin (EPO, a protein secreted by the kidney that stimulates bone marrow red blood cell production) supplementation is very effective in raising hemoglobin. [Author’s Note: Of course this is a WADA banned substance!]
So for most runners, I think time worrying about hemoglobin levels is better spent elsewhere. However, the studies you refer to above, in which performance increases with iron supplementation in patients without overt anemia, are very interesting. I think they show that some athletes have a hemoglobin in the low-normal range, but their bodies ‘want’ the level to be a little higher. It is not easy identifying these patients, but it would require all the blood tests mentioned above, and perhaps an EPO level (a very elevated EPO level would show that the body is ‘trying’ to raise the hemoglobin level).
iRunFar: Are there any additional remarks you would like to make about testing for iron deficiency and anemia? Are there additional tests that would be helpful?
Rasmus Høeg: I think the best way to look at iron studies is to realize that not one test is the perfect test. Well, in fact, that is incorrect. The ‘gold standard’ to diagnose iron deficiency is a bone-marrow biopsy, where a piece of bone marrow is examined for iron content. The bone marrow is where red blood cells are produced, as some readers may know. The problem is that bone-marrow biopsies hurt, so they are usually only done when a cancer of the bone marrow is suspected.
Other tests that may be useful to diagnosed iron-deficiency anemia are:
- Reticulocyte count – A measure of the body’s production of red blood cells. Should be low in iron-deficiency anemia.
- Soluble transferrin receptor – A measure of the body’s attempt to get more iron. Should be high in iron deficiency.
- EPO level – A measure of the body’s attempt to raise hemoglobin levels. A fun to test to get back, but normal levels are not well-defined. Should be high in most types of anemia, but could also be elevated in states of low iron and low-normal hemoglobin.
- There are also some hints in the way the red blood cells look in the microscope that give clues about iron deficiency, but that’s probably too far in the weeds for this article.
That’s a lot of tests! Interpreting anemia can sometimes be like reading tea leaves, and often the doctor will simply start a treatment based on an educated guess and follow the patient closely.
iRunFar: Is there anything else you think readers of this article should know about iron deficiency, iron-deficiency anemia, or anemia in general?
Rasmus Høeg: I think most men can live a long life and not worry about iron deficiency. In fact, if they are diagnosed with iron-deficiency anemia, the least of their worries should be how to run faster. It should be, “Where am I bleeding from?!” In many cases, iron-deficiency anemia in a man should elicit a colonoscopy, upper endoscopy, and urinalysis to look for the cause of blood loss.
For menstruating women, for all the reasons mentioned above, it makes sense to check iron studies periodically, especially at times of fatigue, anemia symptoms, pregnancy, heavy menses, and more.
Call for Comments
- Are you a runner who has developed anemia due to a cause other than a known bleeding source?
- Do you have puzzling labs from an anemia work-up that you would like to share?
- Have you developed iron excess from supplementation or diet? Did you have symptoms from this?
Appendix
Lab-test definitions:
- Ferritin (ng/mL) – Stores of iron in the liver. Low in iron deficiency. High during inflammation.
- Hemoglobin (g/dL) – Amount of hemoglobin (the oxygen-carrying molecule) in the blood. Low in anemia.
- Iron (ug/dL) – The element and its amount per unit blood.
- TIBC (ug/dL) – Total iron-binding capacity, or the amount of room there is for extra iron. This is high in iron-deficiency anemia.
- TS (%) – Total iron saturation or the percent of iron stores that are full.
- Red blood cells (x10E6/µL) – The amount of blood cells per unit blood.
- Hematocrit (%) – The percentage of blood cells per unit blood. Low in anemia.
- MCV (fL) – Mean corpuscular volume, the size of the red blood cell.
- MCHC (g/dL) – Mean corpuscular hemoglobin concentration or the amount of hemoglobin per red blood cell. Low in iron deficiency and vitamin B12 deficiency.
- RDW (%) – Red blood cell distribution width, the percent difference in the sizes of red blood cells. Increased when lots of new blood cells are being made.
- Platelets (thousands/uL) – Number of platelets per unit blood. Unrelated to anemia and iron deficiency.
References
Alfrey CP, Rice L, Udden MM, Driscoll TB (1997) Neocytolysis: physiological down-regulator of red-cell mass. Lancet 349: 1389–1390.
Baska RS, Moses FM, Graeber G, Kearney G. Gastrointestinal bleeding during an ultramarathon. Dig Dis Sci. 1990;35:276–279.
Bastide NM, Chenni F, Audebert M, Santarelli RL, Tache S, Naud N, Baradat M, Jouanin I, Surya R, Hobbs DA, Kuhnle GG, Raymond-Letron I, Gueraud F, et al. A central role for heme iron in colon carcinogenesis associated with red meat intake. Cancer Res. 2015;75:870–879.
Burden RJ, Morton K, Richards T, et al Is iron treatment beneficial in, iron-deficient but non-anaemic (IDNA) endurance athletes? A systematic review and meta-analysis. Br J Sports Med 2015;49:1389-1397.
Cardinale DA, Larsen FJ, Schiffer TA, et al. Superior Intrinsic Mitochondrial Respiration in Women Than in Men. Front Physiol. 2018;9:1133. Published 2018 Aug 17. doi:10.3389/fphys.2018.01133
Chang CC, Chen Y, Modi K, Awar O, Alfrey C, et al. (2009) Changes of red blood cell surface markers in a blood doping model of neocytolysis. J Investig Med 57: 650–654.
Choi SJ, Kim YS, Chae JR, et al. Effects of ranitidine for exercise induced gastric mucosal changes and bleeding. World J Gastroenterol. 2006;12(16):2579-83.
Clénin G. E. 2017. The treatment of iron deficiency without anaemia (in otherwise healthy persons). Swiss Med. Wkly 147:w14434.
Coates A, Mountjoy M, Burr J. Incidence of iron deficiency and iron deficient anemia in elite runners and triathletes. Clin J Sport Med. 2016.
de Benoist B et al., eds. Worldwide prevalence of anaemia 1993-2005. WHO Global Database on Anaemia Geneva, World Health Organization, 2008.
DeRuisseau KC, Cheuvront SN, Haymes EM, Sharp RG. Sweat iron and zinc losses during prolonged exercise. Int J Sport Nutr Exerc Metab. 2002;12(4):428–437. doi: 10.1123/ijsnem.12.4.428.
Dressendorfer RH , Wade CE , Frederick EC. .Effect of shoe cushioning on the development of reticulocytosis in distance runners. Am J Sports Med 20: 212-216, 1992.
Diallo A, Deschasaux M, Partula V, Latino-Martel P, Srour B, Hercberg S, Galan P, Fassier P, Gueraud F, Pierre FH, Touvier M. Dietary iron intake and breast cancer risk: modulation by an antioxidant supplementation. Oncotarget. 2016;7:79008–79016.
Etemadi A, Sinha R, Ward MH, et al. Mortality from different causes associated with meat, heme iron, nitrates, and nitrites in the NIH-AARP Diet and Health Study: population based cohort study. BMJ. 2017;357
Franco RS (2009) The measurement and importance of red cell survival. Am J Hematol 84: 109–114.
Garvican LA, Saunders PU, Cardoso T, Macdougall IC, Lobigs LM, et al. (2014) Intravenous iron supplementation in distance runners with low or suboptimal ferritin. Medicine and science in sports and exercise 46: 376–385.
Gibson RS. Principles of nutritional assessment. Second Edn New York, NY: Oxford University Press, 2005.
Goodnough LT, Nemeth E, and Ganz T. (2010) Detection, evaluation, and management of iron-restricted erythropoiesis. Blood 116(23):4754–4761.
Le CHH. “The Prevalence of Anemia and Moderate-Severe Anemia in the US Population (NHANES 2003-2012)” PloS one vol. 11,11 e0166635. 15 Nov. 2016, doi:10.1371/journal.pone.0166635
Mahlknecht, U. & Kaiser, S. (2010). Age-related changes in peripheral blood counts in humans. Experimental and Therapeutic Medicine, 1, 1019-1025.
Martens P, Nijst P, Verbrugge FH, Smeets K, Dupont M, Mullens W. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol. 2018;73:115–23
Maughan RJ, Burke LM, Dvorak J, et al. IOC consensus statement: dietary supplements and the high-performance athlete. Br J Sports Med. 2018;52(7):439-455.
McCabe ME, III, Peura DA, Kadakia SC. Gastrointestinal blood loss associated with running a marathon. Digestive Diseases and Sciences. 1986;31(11):1229–
McInnis MD, Newhouse IJ, von Duvillard SP, et al. The effect of exercise intensity on hematuria in healthy male runners. Eur J Appl Physiol Occup Physiol. 1998;79:99–105.
Mercer KW, Densmore JJ. Hematologic disorders in the athlete. Clin Sports Med. 2005;24:599–621
Mettler S, Zimmermann MB. Iron excess in recreational marathon runners. Eur J Clin Nutr2010;64:490–4.
Miller B, Pate RR, Burgess W. Foot impact force and intravascular hemolysis during distance running. Int J Sports Med. 1988;9:56–60.
Murphy W. G. (2014). The sex difference in haemoglobin levels in adults – mechanisms, causes, and consequences. Blood Rev. 28 41–47. 10.1016/j.blre.2013.12.003
Ostojic SM & Ahmetovic Z. Weekly training volume and hematological status in female top-level athletes. Ahmetovic Journal of Sports Medicine and Physical Fitness; Sep 2008; 48, 3; ProQuest Nursing & Allied Health Source pg. 398
Otto JM, Montgomery HE, Richards T. Haemoglobin concentration and mass as determinants of exercise performance and of surgical outcome. Extrem Physiol Med. 2013;2(1):33. Published 2013 Nov 26. doi:10.1186/2046-7648-2-33
Ottomano C, Franchini M. Sports anaemia: facts or fiction?. Blood Transfus. 2012;10(3):252-4.
Parks, RB, Hetzel SJ, Brooks MA. Iron Deficiency and Anemia among Collegiate Athletes: A Retrospective Chart Review. Medicine & Science in Sports & Exercise 2017; 49(8): 1711–1715.
Reardon TF, Allen DG. Iron injections in mice increase skeletal muscle iron content, induce oxidative stress and reduce exercise performance. Exp Physiol. 2009;94(6):720–30.
Rice L, Ruiz W, Driscoll T, Whitley CE, Tapia R, et al. (2001) Neocytolysis on descent from altitude: a newly recognized mechanism for the control of red cell mass. Ann Intern Med 134: 652–656.
Rice L, Alfrey CP (2005) The negative regulation of red cell mass by neocytolysis: physiologic and pathophysiologic manifestations. Cell Physiol Biochem 15: 245–250.
Roecker L, Meier-Buttermilch R, Brechtel L, et al. Ironregulatory protein hepcidin is increased in female athletes after a marathon. Eur J Appl Physiol. 2005;95:569–71.
Roy CN, Snyder PJ, Stephens-Shields AJ, et al. Association of Testosterone Levels With Anemia in Older MenA Controlled Clinical Trial. JAMA Intern Med. 2017;177(4):480–490.
Schrier SL &Auerbach M. Causes and diagnosis of iron deficiency and iron deficiency anemia in adults. Uptodate.com. Written 10/2018 and updated 11/2018.
Semedo RM, Santos MM, Baião MR, Luiz RR, da Veiga GV. Prevalence of anaemia and associated factors among children below five years of age in Cape Verde, West Africa. J Health Popul Nutr. 2014;32(4):646-57.
Soppi ET. Iron deficiency without anemia – a clinical challenge. Clin Case Rep. 2018;6(6):1082-1086. Published 2018 Apr 17. doi:10.1002/ccr3.1529
Telford R, Sly GJ, Hahn AG, et al. Footstrike is the major cause of hemolysis during running. J Appl Physiol. 2003;94:38–42.
Terink R, Ten Haaf D, Bongers CWG, et al. Changes in iron metabolism during prolonged repeated walking exercise in middle-aged men and women. Eur J Appl Physiol. 2018;118(11):2349-2357.
Thomas DT, Erdman KA, Burke LM. American college of sports medicine joint position statement. Nutrition and athletic performance. Med Sci Sports Exerc 2016;48:543–68.
Weight LM , Byrne MJ , Jacobs P. .Haemolytic effects of exercise. Clin Sci (Lond) 81: 147-152, 1991.
Woods A, Garvican-Lewis LA, Saunders PU, et al. Four weeks of IV iron supplementation reduces perceived fatigue and mood disturbance in distance runners. PLoS One. 2014;9(9):e108042. Published 2014 Sep 23. doi:10.1371/journal.pone.01080420