You’ve likely heard the adage, “Don’t try anything new on race day.” But if you’ve run a long ultramarathon, you’ve probably also experienced having to throw nutrition plans A, B, and C out the window, which leaves you, well, trying something new. I personally have discovered the wonders of a mile-80 quesadilla when nothing else tasted good, and run on banana halves and Coke because my stomach was doing what felt like backflips. More often than not, it is your nutrition strategy that goes wrong when you’re racing.
The reason why is multifactorial, but simply put, your gastrointestinal (GI) tract is incredibly complex and chock-full of individual nuances which can make it your secret weapon and worst enemy. In fact, one out of every two to three runners experience GI distress during training and/or racing (1). So how do you make sure GI distress doesn’t stop you in your tracks? In this article, we discuss how our incredible GI system works in general as well as during training and races. With this article, we aim to provide you with the tools to train and fuel your gut so that come race day you don’t spend half of your race in the bushes.

Figure 1. Author Corrine Malcolm enjoying a mid-race popsicle with her crew during the 2017 Leadville Trail 100 Mile, her first 100 miler. Photo: Kayla Dalle
Follow the Food: The Gastrointestinal Tract and How it Works
The importance of carbohydrates in endurance-sports performance has long been established in the scientific literature, and becomes particularly important when we run past the two-hour mark (6). However, the journey of the carbohydrate from your lips to becoming effective fuel for your working muscles is not so simple.
Your GI tract is a massive, winding system that starts at your mouth, includes your pharynx, esophagus, stomach, small intestine, large intestine, and finally makes it all the way to your anus. (The final is something I never thought I would type in a publication.) For the purpose of this article, the most important features are the stomach and small intestine as they are the two most crucial digestion and absorption organs.
Digestion is the process of breaking down complex food into much smaller pieces, including water-soluble molecules that your body absorbs in different places in the GI tract. Two main forms of digestion occur, mechanical (or the physical breaking apart of food) and chemical digestion (which involves chemical enzymes to help break the food down to the molecular level). Mechanical digestion primarily takes place in the stomach but also continues all the way to the end of the line. Chemical digestion starts on a small scale in the stomach and finishes in the small intestine where incredible amounts of nutrient absorption takes place.
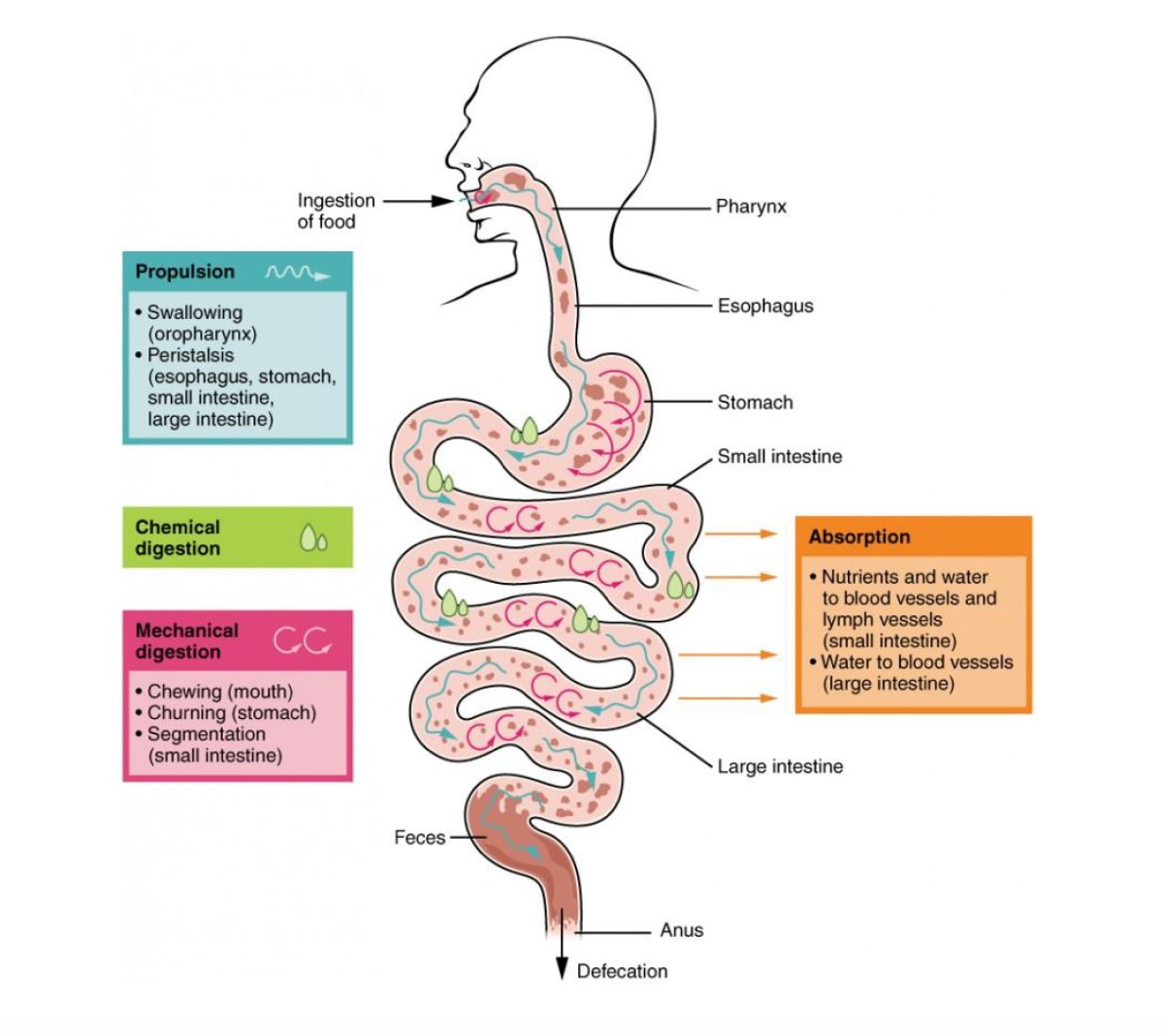
Figure 2. Digestion and absorption through the gastrointestinal (GI) tract has several steps from the time food enters your mouth to when it is absorbed in your intestines. Image courtesy of Alevelbiology.co.uk.
Humans, on average, have 21 feet of (really cool) small intestine! Additionally, the small intestine is lined with villa, or tiny finger-like projections, that increase your small intestine’s surface area, making it the literal hotbed for molecular absorption. Once carbohydrates are broken down into their molecular form, they are called monosaccharides–specifically glucose, galactose, and fructose (which are all simple sugars). These monosaccharides move across your small intestine’s cell membrane (lining) via transporters, into your circulatory system, and on to your muscles. Transporters are exactly what they sound like: they physically carry these molecules across the small intestine’s cell membrane.
The transporter thought to be responsible for the vast majority of ingested sugar absorption is the sodium-dependent glucose and galactose transporter (SGLT1) (2). What’s interesting about SGLT1 is that, as its name suggests, it’s also the transporter for sodium across the small intestine’s cell membranes, which influences hydration status and sodium blood-serum levels. Essentially SGLT1 works double duty.
Fructose, or the sugar commonly associated with fruit, has its own transporter, glucose transporter 5 (GLUT5) (2). This is why even when your body has reached its maximum capacity for absorbing carbohydrates in the form of glucose or galactose, the body can continue to absorb fructose.
The final transporter is glucose transporter 2 (GLUT2). GLUT2 is the primary glucose transporter between our liver and blood, however, GLUT2 is also found in the small intestine and when it senses that the body is in a fed-state it will upregulate and enhance the capacity for glucose to be transported into the bloodstream.
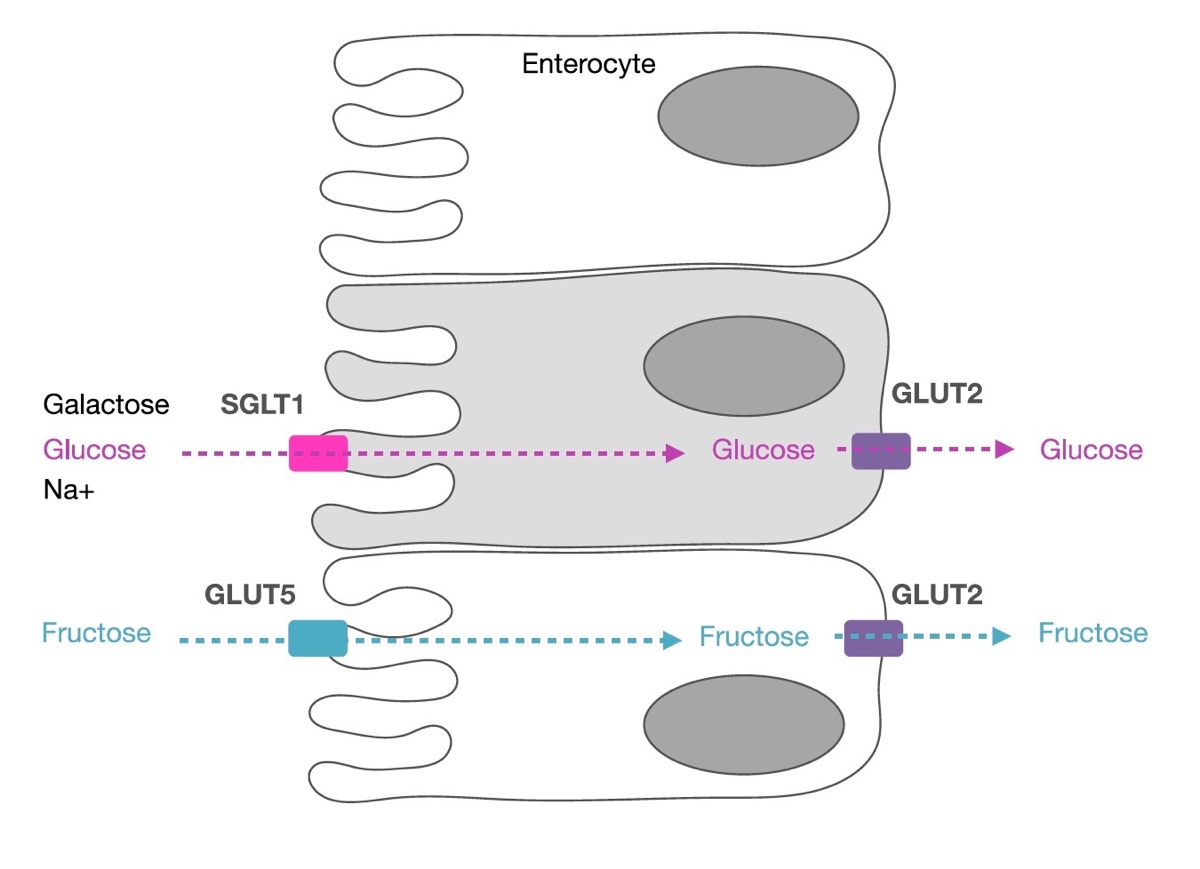
Figure 3. Galactose and glucose utilize co-transport to cross the small intestine’s cell membrane with sodium via the sodium-dependent glucose transporter 1 (SGLT1). Fructose is transported via glucose transporter 5 (GLUT5) which is not sodium dependent and is highly specific to fructose. All three use glucose transporter 2 (GLUT2) to be transported into the circulatory system. For your information, enterocytes are cells making up the intestine’s lining. Image courtesy of Asker Jeukendrup, 2017 (2).
When you put it all like this, digestion and absorption seems pretty straightforward. Eat food, make food so small it’s microscopic, piggyback transporters to move food molecules from our small intestines into our blood circulation. Unfortunately, despite having feet upon feet of digestive surface area, the system is still fickle (but trainable!) at best. With carbohydrate intake, there is a complex interaction between numerous other factors such as the macronutrient makeup of your day-to-day diet (how many grams of carbohydrates you normally consume), environmental conditions (like heat and high altitude), sport type (stress from jostling of running, for example), the concentration of carbohydrate solution you’re consuming (which we will discuss in just a little bit), the types of carbohydrates being consumed, and even the carbohydrate source’s acidity (1).
Bloating and Other Unmentionables: The Basics of GI-Tract Distress
There are four main causes of GI-tract distress:
- Volumetric discomfort or upper GI issues (you have too much liquid and/or food in your stomach);
- Splanchnic hypoperfusion (there’s decreased blood supply to the tissues and organs of the GI tract);
- Decrease in enteric nervous-system activity (there’s decreased GI tract nervous-system activity; this is not fully understood but essentially it seems like there is a decrease in ability for food to move through the system because of decreased neural activity); and
- Nutritional-intake hindrance (you’re eating too little, too much, or the wrong kinds of food) (6).
Some symptoms of GI distress are inconvenient and/or performance limiting; it’s hard to win a race from the inside of a port-o-potty. But other GI symptoms are more serious and can lead to longer-term health implications including impacting how your gut absorbs nutrients and minerals and the potential for microscopic blood loss in your stool (which would in turn have larger impacts on anemia-prone individuals). Milder symptoms include bloating and flatulence, whereas more serious symptoms include mucosal erosion and ischemic colitis (acute damage and inflammation to the GI-tract lining and injury to the large intestine/colon due to lack of blood supply which can cause post-event blood loss via your stool) (1).
The most common symptoms of GI distress in runners competing in races 67 to 161 kilometers in length are nausea, abdominal cramps, diarrhea, and vomiting. In a study looking at two different 100-mile races, the most common reasons for dropping out were nausea and/or vomiting, and it was the second-most-common problem impacting the race-day performances among finishers in the study (3). Clearly GI distress can be a day-ender when it comes to finishing an ultramarathon.
Why is This Happening to Me: Digging Deeper into GI Distress
Bloating, belching, and regurgitation are the most commonly reported symptoms of upper-GI distress and are thought to be caused by volumetric overload, or taking in a larger volume of liquids and solids than what your GI tract is used to. This physically ‘stretches’ the stomach and causes discomfort (6). Think about competitive eaters: they don’t absorb any more food than normal people; rather they physically ‘fit’ more food into their stomachs. The same can be said for runners. Studies involving trained runners have shown that repeated food challenges over a two-week period (this can even be consistent or slightly more intake than usual of plain fluids) creates a significant decrease in gut discomfort and upper-GI distress symptoms during subsequent runs and races (6, 1, 2).
Maybe the largest known contributor to GI distress is called splanchnic hypoperfusion, which can be anything from a mild change in blood circulation in the GI tract’s tissues to a more extreme GI ischemia, or a total lack of blood supply (1,6). During exercise, blood flow to your GI tract normally reduces by up to 80% as compared to being at rest (8). This is because blood is being shunted away from the gut to the active muscles and skin. More blood goes to your muscles during exercise to deliver oxygen to them, and more blood goes to the skin to help dissipate the heat generated by exercise. This process can become more extreme in hot weather when more heat dissipation by the skin is needed and at altitude when your working muscles require more oxygen (1).
When blood is shunted away from the GI tract for an extended period of time during hard exercise, like while running an ultra, you can sustain a ‘gut injury.’ This gut injury causes a change in the permeability and function of the small intestine’s cell membrane, or how carbohydrate transporters (SGLT1, GLUT5, and GLUT2) function. The most common symptoms of splanchnic hypoperfusion are nausea, vomiting, abdominal pain, diarrhea, and iron loss through microscopic GI bleeding (1).
Most of these symptoms are short lived and improve as blood supply returns to the GI tract. However, just like any other injury, inflammation is not short lived, and similar to your sore quadriceps post-ultra, it can take a couple of days to weeks for that inflammation to go away completely. The biggest impact of inflammation is malabsorption of nutrients and minerals post-race as your gut heals, so take good care of yourself after you cross the finish line. Avoid eating foods that are hard to digest such as processed and high-fiber foods because they irritate your gut; focus on foods that reduce inflammation and restore your gut bacteria such as fermented foods, good fats, and bone broth; sleep a lot; stay hydrated; and consider supplementing with probiotics and fish oil.
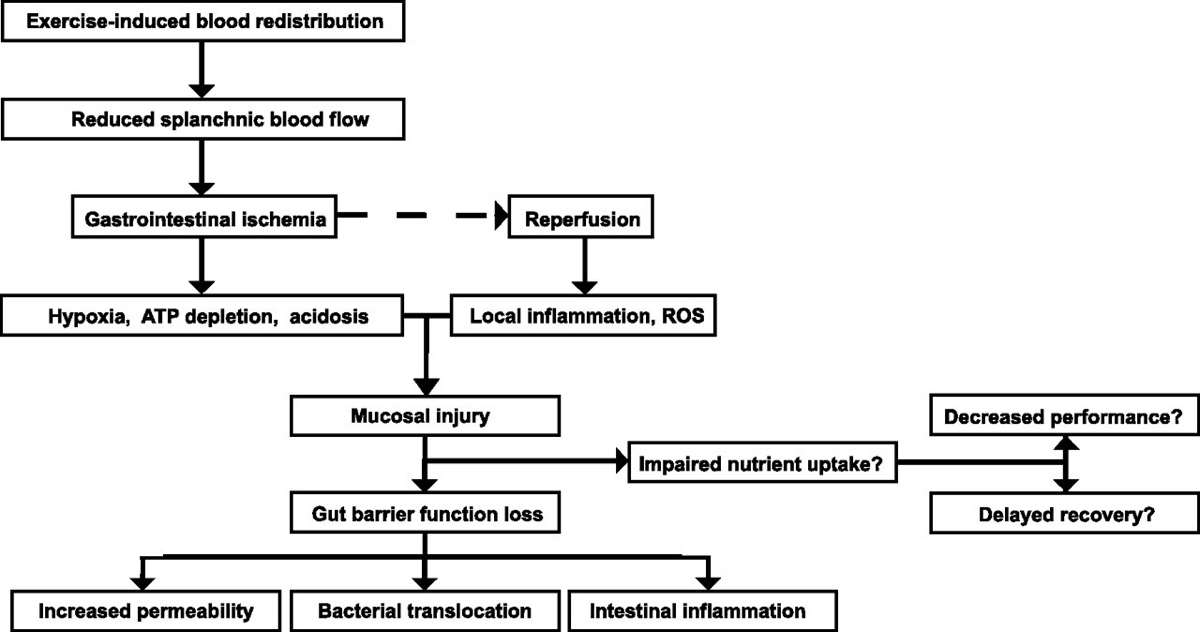
Figure 4. Hard exercise leads to a reduction in blood flow to your GI tract, or splanchnic area. Ischemia, a lack of blood supply, leads to hypoxia, a lack of oxygen, and causes damage to that tissue. This causes injuries to your stomach and small intestine which can affect the gut’s ability to absorb nutrients. Some of the function returns with the return of blood flow, or reperfusion, but other functions do not completely recover until inflammation returns to normal, or resting, levels. Some more definitions to note: ATP depletion is a lack of an energy source, acidosis is an acidic gut, ROS is reactive oxygen species, mucosal injury is an injury to the mucus membrane of the GI tract’s organs, increased permeability is issues with transporters, and bacterial translocation affects your microbiome. Image courtesy of Van Wijck K, Lenaerts K, Grootjans J, Wijnands KAP, Poeze M, van Loon LJC, Dejong CHC, & Buurman WA. Physiology and pathophysiology of splanchnic hypoperfusion and intestinal injury exercise: strategies for evaluation and prevention (8).
The other significant factor, and maybe the thing we can influence the most, is how our own nutritional strategies work for and against us. Some of this is influenced by our day-to-day nutritional habits, and the other piece is our caloric intake on the run.
Things that we know can cause GI distress and even ’emergencies’ on the run include diets that are high in fiber, fat, protein, and fructose as they all alter the gastric-emptying rate, which means they slow or speed food’s passage through your GI tract (1). Foods that are high in fat can cause gastroparesis, or ‘stomach paralysis,’ and slow the rate at which food leaves the stomach. Foods high in fiber result in similar issues but additionally can cause blockages in the stomach called phytobezoars made from the indigestible food fibers like cellulose. On the other hand, foods that move through the stomach more quickly include liquids and simple carbohydrates because they take much less time to digest into small-enough molecules to be absorbed in the small intestine.
Additionally, carbohydrate oxidation, or your ability to utilize the carbohydrates you ingest, is directly related to your daily carbohydrate intake. This is because the more carbohydrates you eat (moderate to high levels in your diet) the more SGLT1 transporters you have readily available in your small intestine. Remember, SGLT1 is the key transporter in moving glucose and galactose from your small intestine into your bloodstream. This might not sound like a big issue, as you oxidize other macronutrients for energy after all. But if you eat a low-carbohydrate diet regularly and try to only up your carbohydrate intake during a race, you do not have the transporters needed to move glucose into your circulatory system and to your active muscles. This is important because despite how well you oxidize fat you still utilize and only have a finite amount of carbohydrates stored in your body, so if you cannot absorb enough ingested carbohydrates you will eventually ‘overdraw’ your carbohydrate bank account.
This is also the same reason we should practice our race-day fueling strategy during our long training runs. The stomach and small intestine are trainable organs. Studies have shown that even three days of moderate-high carbohydrate intake is enough to upregulate your SGLT1 transporters (2). This would best be implemented on your intensity and long-run days when your body needs carbohydrates the most and at times that are most analogous to race day, at a minimum of four to six weeks before a goal race.
The other major cause of dietary-related GI distress is strongly linked to osmolality, or in this case concentration of the solution (the combination of all food and liquid) you consume. This is might be the most common race-day mistake. An osmolality issue could be from either the concentration of the beverage you ingest or a combination of the food (gels, bars, oatmeal cream pies) and fluid you take in.
Osmolality is important because hydration (and secondarily absorption of nutrients in your small intestine) relies on concentration gradients, or the moving of solutes (the solids in a solution) from an area of higher concentration to an area of lower concentration. In the case of nutrient movement, we are comparing the ingested solution (which includes all solids such as carbohydrates, electrolytes, branched-chain amino acids, flavorings, and more) to the concentration of our blood. Our bodies’ fluids have a natural concentration of about 280 to 300 mosm/kg (milli osmoles or solute per kilogram or liter of water). If we ingest something more concentrated than that, instead of hydrating and fueling ourselves, we instead pull water out of our body’s fluids and into our small intestine, causing GI distress and dehydrating ourselves in the process. This most commonly happens when we add whole-food calories or sports foods on top of higher-calorie sports drinks.
For most efficient absorption, ingest a solution that is roughly equal to the body’s natural blood concentration. If that sounds complicated, it is, sort of. But this is where running nutrition comes into play, as numerous endurance-nutrition companies have created products specifically containing optimal concentrations. Read on to learn more about this.
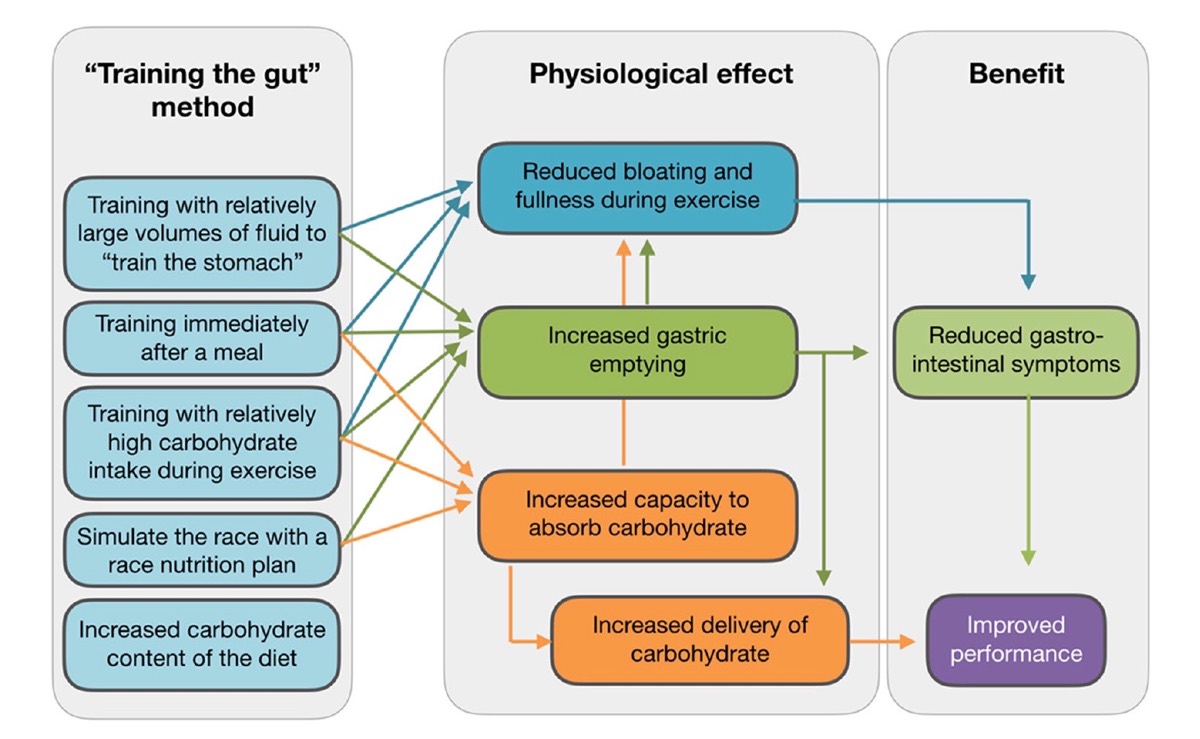
Figure 5. The methods of gut training and their positive physiological effects and subsequent performance improvement. Image courtesy of Asker Jeukendrup, 2017 (2).
How to Win the Eating Competition at Your Next Ultramarathon
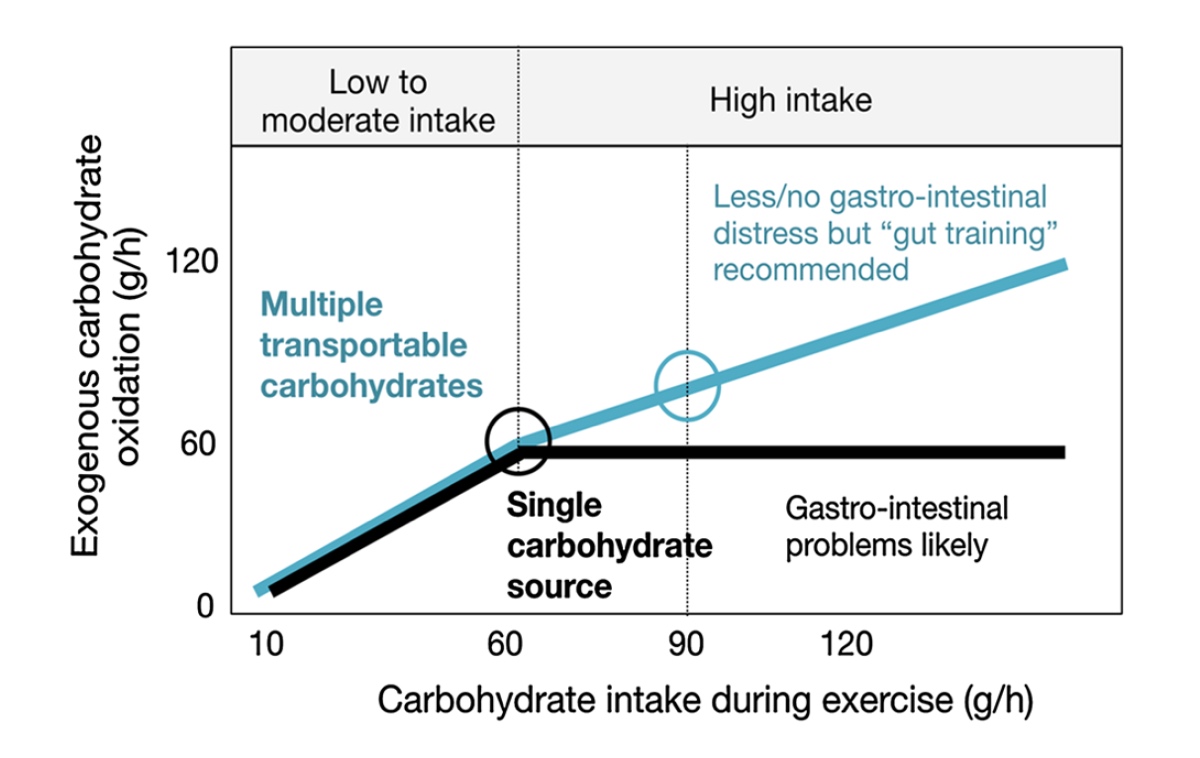
- Utilize a mixed-carbohydrate approach. It’s believed right now that the upper limit of your ability to ingest carbohydrates via one source and likely glucose is approximately 60 grams/hour. For your reference, GU Energy Gels contain 20 to 23 grams/gel, CLIF Shot Energy Gels contain 22 to 24 grams/gel, and Spring Energy Gels contain 12 to 20 grams/gel. Going much above that 60 grams of carbohydrates per hour from a singular carbohydrate source (all glucose) can lead to GI distress. However, if you combine glucose with another carbohydrate like fructose, you can ingest up to a combined total of about 90 grams of carbohydrates per hour (2). Use caution and self-experiment (preferably before race day) as too much of anything can be bad and 30 to 40% of people can have fructose malabsorption which will have you rushing to the bushes. Your body doesn’t know the difference between gels, chews, chomps, bars, and liquid calories. True, liquids and gels move through your GI tract more quickly because they take less mechanical breaking down, but everything is broken down into its individual parts and processed through the stomach and small intestine. The most common mistake is simply creating a solution that is too concentrated. If you need solid foods to help maintain that satiated feeling, I recommend ingesting them with water instead of a medium- or high-calorie drink.
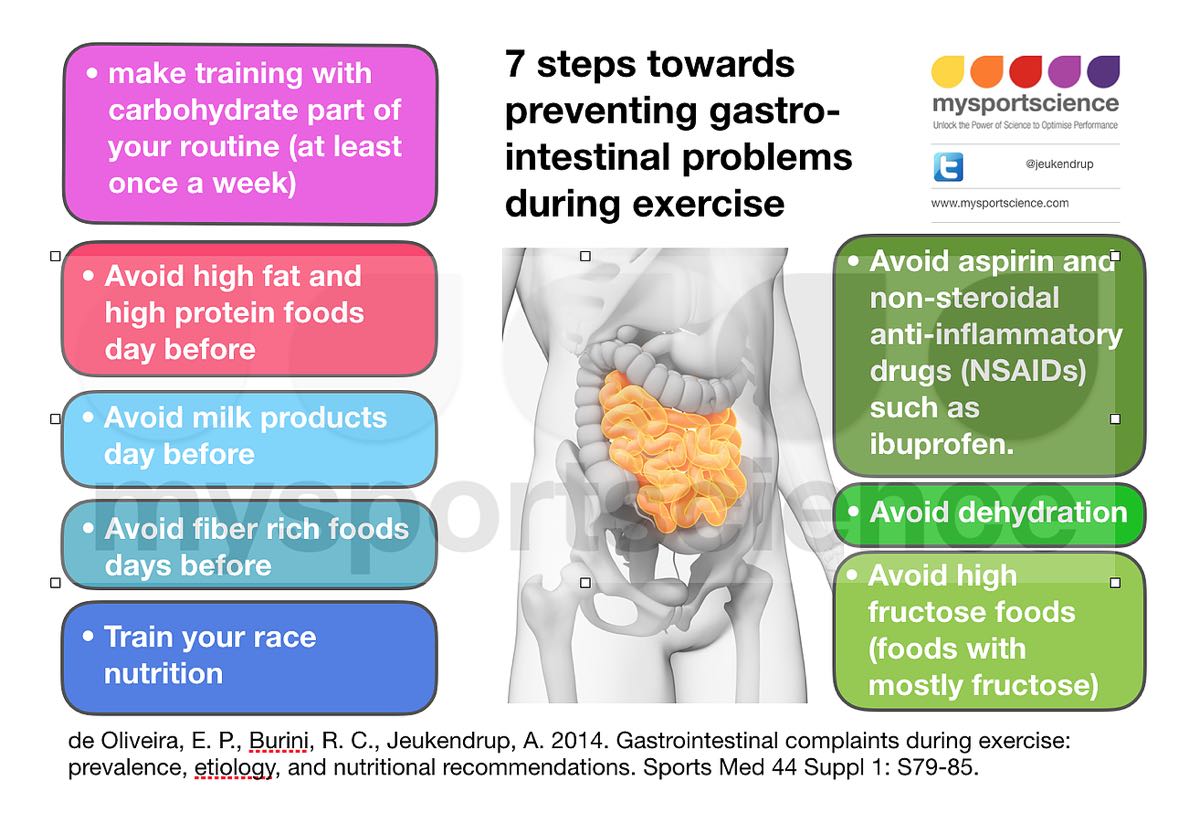
- Avoid prolonged dehydration. Shifts in concentration gradients inhibit your body’s ability to transport both fluids and nutrients from your small intestine to your bloodstream and therefore your muscles.
- Avoid unnecessary ibuprofen use. Ibuprofen has been shown to aggravate exercise-induced small-intestine injury, increase rates of gut-barrier dysfunction, and can lead to increased risks of upper GI issues and mucosal bleeding (caused by ischemia-induced gut injury). Athletes who experience persistent or recurring GI symptoms should consider avoiding use of non-selective non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, Aleve, and Aspirin (1,4,5).
- Avoid consuming high amounts of fiber, protein, fat, or fructose before and during your run as this food leaves the stomach generally more slowly or quickly and can lead to GI distress.
- Practice your race-day nutrition plan. This means practicing how many grams of carbohydrates you consume per hour and preparing to troubleshoot on race day. Create an aid station during your long training efforts to practice your Coke, quesadilla, and potato-chip habit.
- Train in adverse conditions and the conditions in which you will race, such as in the heat or at altitude. Different environmental conditions create new demands on your GI tract and require tweaking your nutritional needs and practices. Practice makes… for better prep!
- Give yourself enough time to have a normal bowel movement before racing, and if not be prepared to carry some toilet paper, dig yourself a hole (of the literal variety), and pack out your used toilet paper.
- Prepare for the worst. It might involve a puke and rally or a rest break, but you can reset your stomach following GI distress. Give yourself permission to slow down so blood can return to your gut, sit down and eat some solids, or nurse some liquid calories. Don’t let a rough patch ruin your day!

Figure 6. Carbohydrate quantity and type and their effects on potential GI-tract distress. Mixed carbohydrates (glucose and fructose) allow for higher carbohydrate uptake with less risk of GI distress. Exogenous carbohydrate oxidation is carbohydrates ingested as opposed to using carbohydrates stored in your muscles and liver. Image courtesy of Asker Jeukendrup, 2017 (2).
Call for Comments (from Meghan)
- What has been your most successful nutritional strategy for shorter trail races, and what about your longer ultramarathons?
- Can you share an example of a time when your nutrition went wrong in a race, what you think happened, and if and how you were able to recover?
- What nutritional tips and tricks work for you?
References
- de Oliveira EP, Burini RC, Jeukendrup A. Gastrointestinal complaints during exercise: prevalence, etiology, and nutritional recommendations. Sports Med. 2014;44:S79–85.
- Jeukendrup A. Training the Gut for Athletes. Sports Med (2017) 47 (Suppl 1): S101–S110 DOI 10.1007/s40279-017-0690-6
- Hoffman MD, Fogard K. Factors related to successful completion of a 161-km ultramarathon. Int J Sports Physiol Perform. 2011;6:25–37.
- Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med. 1991;115:787–96.
- van Wijck K, Lenaerts K, van Bijnen AA, et al. Aggravation of exercise-induced intestinal injury by Ibuprofen in athletes. Med Sci Sports Exerc. 2012;44:2257–62.
- Costa R, Miall A, Khoo A, Rauch C, Snipe R, Camoes-Costa V, & Gibson P. Gut-training: The impact of two weeks repetitive gut-challenge during exercise on gastrointestinal status, glucose availability, fuel kinetics, and running performance. Applied Physiology, Nutrition, and Metabolism. 2017. apnm-2016-0453.R4
- Jeukendrup A. A Step Towards Personalized Sports Nutrition: Carbohydrate Intake During Exercise. Sports Med. 2014; 44(Suppl 1): 25-33. doi: 1007/s40279-014-0148-z
- Van Wijck K, Lenaerts K, Grootjans J, Wijnands KAP, Poeze M, van Loon LJC, Dejong CHC, & Buurman WA. Physiology and pathophysiology of splanchnic hypoperfusion and intestinal injury exercise: strategies for evaluation and prevention. American Journal of Physiology. 2012: 303 (2). https://doi.org/10.1152/ajpgi.00066.2012
- Fedewa A & Rao S. Dietary fructose intolerance, fructan intolerance and FODMAPs. Current Gastroenterology Reports. 2014 Jan: 16(1): 370. doi: 1007/s11894-013-0370-0